This is one of the most dreaded complications that can arise from medical treatment Multiple organ failure. Only about half of the affected patients survive if several organs such as kidneys, lungs or heart fail at the same time.
What is multiple organ failure?

© baluchis– stock.adobe.com
If necessary, the organs can be replaced by machines for a while. If the brain or liver is affected by the failure, the patient can usually no longer be helped. In order to have any chance of survival in the event of multiple failures of various organs, the patient must be treated in intensive care.
However, that occurs Multiple organ failure often only in the intensive care unit. However, there it is usually recognized very quickly. Despite rapid countermeasures, this complication remains one of the most common causes of death in intensive care units.
Multi-organ failure is basically very simply defined. If two or more organs stop working at the same time, this is already a multiple organ failure. However, medical professionals now speak of a multiple organ dysfunction syndrome, or MODS for short.
causes
There are several reasons that lead to one Multiple organ failure being able to lead. The two most important are accidents and bacterial poisoning.
If several organs are injured in an accident, this can lead to a chain reaction that leads to the failure of other organs. The same applies to the dreaded sepsis. This is poisoning that spreads rapidly over the entire body and can lead to severe inflammation everywhere.
Heart disease or allergies can also trigger multiple organ failure. This can be the case if the patient suffers a life-threatening anaphylactic shock, which can paralyze the circulation and various organs. Another cause, however, is simply old age. In a very old and very weakened body, the failure of one organ can quickly bring down the others.
Symptoms, ailments & signs
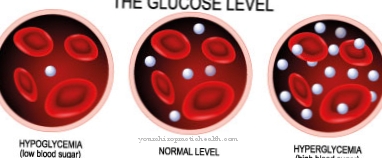
The symptoms of multiple organ failure result from the respective insufficiency of the affected organs. Manifest kidney failure manifests itself in a decrease in the filter performance of the kidneys. More and more urinary substances, water and electrolytes remain in the body. This can lead to overhydration with brain edema, pulmonary edema or heart failure.
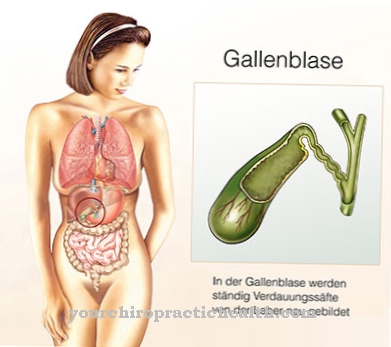
Liver insufficiency is manifested by yellowing of the skin (jaundice) and blood clotting disorders with prolonged bleeding times. Disturbances of consciousness up to a coma can also occur. The patients smell of raw liver (foetor hepaticus) from the mouth and show what is known as flapping tremor.
It is a gross tremor of the hands. Because bile leaks from the liver vessels into the blood, people with liver failure also suffer from itching. This is particularly noticeable on the foot. Rapid breathing and shortness of breath are the main symptoms of acute lung damage.
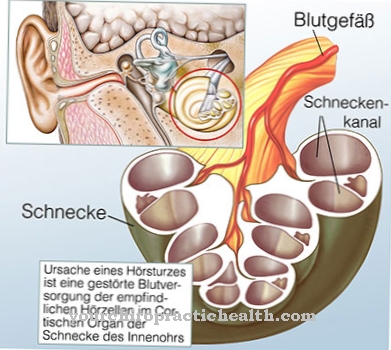
Due to the lack of oxygen supply, the patient's skin turns blue. This is also called cyanosis. Restlessness and confusion are other symptoms that can occur with lung failure. In some patients, a drop in body temperature (hypothermia) or an increase (hyperthermia) up to fever can be observed.
Diagnosis & course
The exact diagnosis of the Multiple organ failure depends of course on which organs are affected. Since this complication mostly occurs in intensive care units, the failure of various organs is usually recognized very quickly and indicated to the nursing and treating staff by technical means. At the moment when multiple organ failures are recognized, action must be taken very quickly, as any delay dramatically reduces the patient's chances of survival.
Complications
Multi-organ failure as a result of a serious illness, infection, shock reactions, allergies or a serious nutrient deficiency is already a complication that increases in severity with the number of failing organ systems. If the functions of individual organs have to be compensated for by intensive medical measures, this is associated with considerable interventions in the patient. Operations and organ removal may be necessary, which again involve their own risks.
The removal of organs leads to a lifelong dependence on machines such as dialysis machines (kidneys) or ventilators (in the event of a malfunctioning lung). Sepsis, which can occur as a result of dead organs and cellular and metabolic toxins released into the body, is particularly dangerous. The poisoning leads to further inflammation and the loss of other organ functions.
In addition, as a result of multiple organ failure or an induced coma in such a case, an oxygen deficiency in areas of the brain can occur. The damage caused is irreversible and then affects the person concerned forever.
If the liver or the brain is affected by sepsis, which occurs in the course of multiple organ failure, the medical measures are exhausted. The same applies to complete liver failure as part of multiple organ failure. Brain death is to be equated with death. The mortality rate increases with the number of failing organs and the sequelae.
When should you go to the doctor?
In the event of multiple organ failure, an emergency doctor must be called immediately or the hospital must be visited directly. If no quick medical treatment is initiated, the multiple organ failure usually leads to the death of the person concerned. The earlier the disease is diagnosed and treated, the greater the chances of recovery. In most cases, however, with multiple organ failure, the patient is already in a hospital or undergoing other medical treatment.
The patients suffer from severe pain, fever, shortness of breath and disorders of consciousness. Often they can no longer walk, eat or drink alone and need help from other people in their everyday lives. If these symptoms occur, a doctor must immediately carry out an examination. Heart failure or kidney failure can also occur. Cyanosis or other breathing difficulties can also indicate multi-organ failure and should be investigated.
The treatment depends heavily on the organs affected and is usually carried out in a hospital. However, it cannot generally be predicted whether this will lead to a positive course of the disease. Often the life expectancy of the person affected is significantly reduced by the multiple organ failure.
Doctors & therapists in your area
Treatment & Therapy
Treating a Multiple organ failure naturally depends on the organs affected, but also on what triggered the complication. For example, if sepsis is the starting point for the organ failure, the focus of inflammation must be identified and eliminated as quickly as possible, and the patient is treated with antibiotics.In the event of severe external injuries, for example due to an accident, the affected organs may need to be mechanically supported or even replaced.
An important tool in the treatment of multiple organ failure is the artificial coma. However, medical professionals prefer the expression "artificial deep sleep". The patient is put into a coma-like state by means of various drugs. This is to protect the brain from the effects of multiple failures of the organs. When the brain is affected, the patient usually cannot be saved.
Brain regions that are affected by MODS, e.g. due to a lack of oxygen, remain irreversibly damaged. Through the artificial deep sleep, all body functions are significantly reduced. Body temperature also drops. This makes it easier for certain parts of the body to regenerate and for affected organs to be better treated and restarted.
Outlook & forecast
If a patient experiences multiple organ failure, the chance of survival is very low. It depends on the restricted or failed organs as well as the possibility of treatment. If multiple organ failure is not treated promptly, death is inevitable. There is no prospect of spontaneous healing or the like. The mortality rate with three failed organs is still around 80 percent, even with medical treatment.
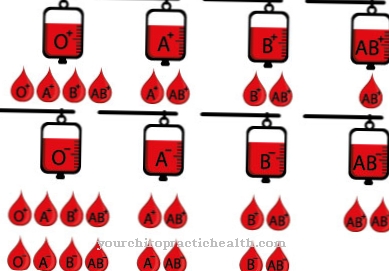
Affected people can be partially stabilized and kept alive in an intensive care unit. How well this works depends on the organs that have failed. For example, it is easier to replace the kidneys and lungs than it is to replace the liver or heart. The failure of the cardiovascular system in particular is almost always fatal. Artificial ventilation can sometimes be maintained for a very long time. A failed gastrointestinal tract can also be compensated for. Since those affected mostly fall into a coma or are put into one in this state, at least the suffering seems limited.
If several organ systems fail, however, even when growing out of a coma, it is often no longer to be expected that those affected will recover well. At best, this would be the case if fewer, ideally non-vital organ systems fail.
prevention
It is difficult to prevent accidents. On the other hand, against infections. 15 percent of all patients in German intensive care units suffer from a so-called nosocomial infection. Behind this is the dreaded “hospital infection”. This can lead to multi-organ failure, especially if the infection was triggered by resistant pathogens.
Therefore, one of the most important preventive measures against multiple failures of the organs is very pronounced and meticulous hospital hygiene. Allergy sufferers, on the other hand, should avoid any situation that could lead to an allergic shock. It is therefore fundamentally important to know exactly about your own possible allergy behavior.
Aftercare
In most cases, multiple organ failure leads to a shortened life expectancy. Then aftercare can only assume a palliative character. Doctors try to counteract the failure of vital organs. Intensive care treatment is indicated. Since there is little time left, pastoral talks play an important role.
If multiple organ failure is survived, consequential damage usually remains. These require long-term treatment. Many patients are dependent on dialysis for the rest of their lives. A normal everyday life is hardly possible. Taking medication is important to relieve the symptoms. Follow-up checks at short intervals are common.
The type of follow-up examination depends on the particular clinical picture. A conversation and a physical examination take place regularly. Blood is also drawn frequently. Imaging procedures regularly support the diagnosis and provide clear conclusions about the course of the disease. Additional outpatient therapies can be prescribed.
If patients belong to the small group of people who do not have any secondary diseases, no follow-up care is necessary in view of the freedom from symptoms. However, experience has shown that many sufferers have problems finding their way back into their everyday lives. Doctors therefore often prescribe sessions with a psychotherapist in order to achieve stabilization.
You can do that yourself
Multiple organ failure is often fatal, even if it occurs in an intensive care unit and doctors have anticipated this dreaded complication. They may put the patient in an artificial coma or remove affected organs, such as the kidneys.
This has consequences for the survivor that have a not inconsiderable impact on their future life. He may need dialysis and / or other therapies for the rest of his life. These therapies should never be left out. This also applies to physiotherapy, which is intended to mobilize the patient again.
To have stood so close to the threshold of death does not leave a patient without a trace. Even if there are no secondary illnesses, the sufferer will struggle to resume their previous life. In any case, he should seek psychotherapeutic treatment. Group therapy with other patients is also advisable. The treating clinics provide addresses and contact persons. Since multiple organ failure is often the complication of sepsis, the website www.sepsis-hilfe.org also offers information and assistance. The reports from those affected who have survived multiple organ failure are particularly helpful here. There is no way to prevent multiple organ failure after an accident or in old age. Sepsis, on the other hand, can be prevented, which at the same time also prevents multiple organ failure.









.jpg)

.jpg)
.jpg)











.jpg)