A Inflammation of the oral mucosa is a reddening of the mucous membranes that occurs in the mouth region and is often perceived as unpleasant. It can be localized or it can extend to the entire inner oral cavity. In the following, the definition, causes, diagnosis, therapy and prevention of oral mucosal inflammation will be discussed in more detail.
What is oral mucosal inflammation?

© Siniehina - stock.adobe.com
The Inflammation of the oral mucosa is also defined in common parlance as mouth rot, or technically as aphthous stomatitis. Since this disease is very often caused by viral infections, especially the herpes virus, the term "herpes simplex type 1" or HSV-1 is also common.
Oral mucosal inflammation is one of the periodontal diseases, i.e. diseases that attack the inner areas of the mouth such as the gums or the oral mucosa.
causes
Inflammation of the oral mucosa are often noticed as side effects of other diseases. The most common direct cause of oral rot is herpes viruses.
It is estimated that around 95% of all people carry the herpes virus, but it remains passive until the immune system is too weakened by other diseases. In most cases, HSV-1 is the cause of the disease, and HSV-2 in isolated cases.
Herpes is highly contagious and mainly affects young children, and in rare cases also adults. It can be transmitted through direct skin contact or through saliva. The incubation time of herpes is a maximum of 26 days, whereby it should be noted that the majority of all infections with such viruses are asymptotic, i.e. there is no outbreak of oral mucosal inflammation.
Symptoms, ailments & signs
The inflammation of the oral mucosa (stomatitis) has a different appearance depending on the causative agent. Most of the time, stomatitis causes only mild to moderate symptoms and remains localized. However, complete infestation of the oral cavity cannot be ruled out and is often the result of a weakened body defense. General characteristics include an intense reddening of the oral mucosa.
Swellings, which can be reminiscent of ulcers in their severity, are also typical. Many of the affected areas give sufferers mild to moderate, sometimes burning pain. Infections with the involvement of the Candida yeast cause striking, white coatings (oral thrush) to develop. Simple scraping with a brush or spoon removes the noticeable deposits.
The surface of the oral mucosa often shows bloody tears in stomatitis. An inhibited flow of saliva aggravates the symptoms and slows down the healing process. The formation of vesicles (canker sores) when infected with a virus is often accompanied by an unpleasant halitosis. These circular, red zones of inflammation have a maximum diameter of five millimeters.
At the same time, they are surrounded by a whitish coating. Herpes viruses can develop a large number of small canker sores. The resulting bad breath is extremely penetrating. The oral mucosal inflammation then turns into oral rot. If the disease progresses seriously, those affected face serious problems eating.
Pain, numbness and difficulty swallowing increase the level of suffering up to complete refusal to eat and lead to further weakening of the patient. In addition, there is a fever, general malaise with vomiting and severe exhaustion.
Diagnosis & course
In those cases in which after the incubation period between 1 and 26 days there is actually a symptomatic Inflammation of the oral mucosa occurs, the following symptoms should be visible:
As the name suggests, the clearest sign of an inflammation of the oral mucosa is the reddish swelling of the mucous membrane that makes up the inside of the mouth. However, this can also affect the deep throat, roof of the mouth, and gums. Cold sores can also form, and lesions and ulcerations can occur in the mouth and also on the lips.
In addition, the lymph nodes in the neck area swell noticeably, bad breath, increased salivation and a slight fever are also unpleasant. Based on this clinical picture and some laboratory tests, a doctor will be able to make a reliable diagnosis of oral mucosal inflammation.
Complications
An inflammation of the oral mucosa usually leads to swallowing and chewing difficulties and as a result to loss of appetite and restricted fluid intake. This can lead to dehydration and malnutrition, among other things. The diverse symptoms such as fever, increased salivation and swelling of the lymph nodes can lead to serious complications if left untreated.
In the long term, inflammation of the oral mucosa leads to gum disease. Periodontitis leads to strong bad breath and in the long term increases the risk of serious illnesses such as heart attack or stroke. It can also lead to teeth shifting and further inflammation, which in turn lead to complications.
In addition to the physical consequences, these side effects often lead to social exclusion and thus to psychological problems. In the chronically ill in particular, the general physical and mental well-being decreases considerably. Typical complications of treatment include side effects from mouthwashes, pain relievers, and anesthetics, and bleeding and scarring after surgery.
Home remedies and natural remedies can also damage the oral mucosa. This can lead to bleeding gums, inflammation of the gums and other complications. Due to the severity of these secondary symptoms, a doctor should be consulted immediately if an inflammation of the oral mucosa is suspected.
When should you go to the doctor?
If the person is suffering from changes in the mucous membranes in the mouth and throat, there is cause for concern. If the abnormalities persist for several days or if they increase in intensity, a doctor should be consulted. In the case of small inflammations, the symptoms may decrease or spontaneous healing may occur within a short period of time. A doctor is usually not needed in these cases. However, if major impairments occur, rapid relief of the symptoms should be initiated through medical treatment.
Exercise increased caution if the taste of blood in the mouth recurs or if pus forms. Open wounds can develop, which in severe cases trigger sepsis. Germs and other pathogens can get into the organism and trigger further illnesses or worsen the general state of health.
A visit to a doctor is advisable in the event of refusal to eat, an increased body temperature or irritability. If you experience unwanted weight loss, bad breath or pain in your mouth, you should consult a doctor. Canker sores or blisters in the mouth, problems with existing dentures or swellings should be examined and treated. If the teeth can no longer be cleaned due to the existing complaints, if there is a headache or sleep disorders, the person concerned needs help.
Treatment & Therapy
When treating Inflammation of the oral mucosa A distinction is made between drug and non-drug treatment, but both of which are usually only aimed at combating the unpleasant symptoms. Because the disease does not pose a fatal danger and over time it subsides by itself.
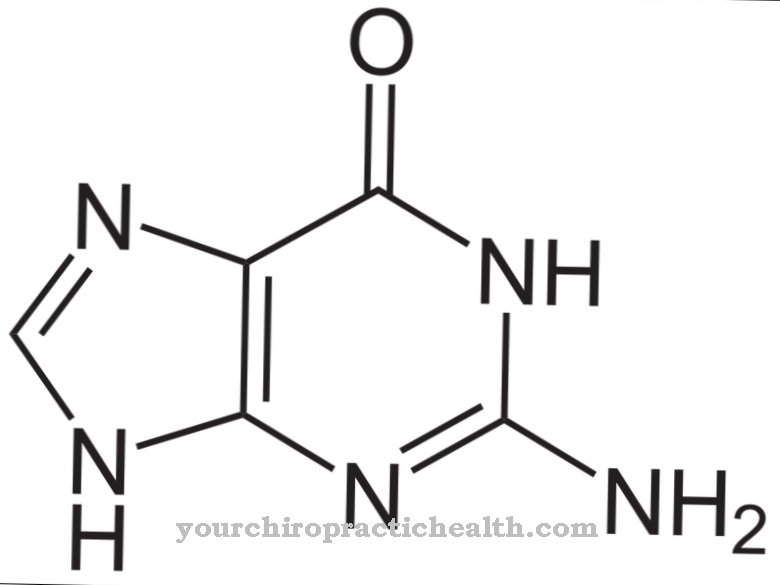
Various pain relievers such as paracetamol or anesthetics can be prescribed to relieve pain in the mouth area. If you decide to actively fight the viruses, nucleoside analogues are usually used, a drug that prevents the viruses from spreading by damaging the viral DNA polymerase. Mouthwashes can also relieve irritation and pain; mixtures of diphenhydramine and antacid are recommended here.
In the case of all medications, however, it is essential to consult a doctor about which medication is also suitable for small children. The non-drug treatments primarily include avoiding dehydration, which is achieved by taking fluids and preferably semi-solid food (porridge, etc.). Care must be taken because children do not like to eat on their own due to the pain when eating and swallowing.
Otherwise, the body will usually heal itself, but the person affected by oral mucosal inflammation, especially if it is a child, should stay at home due to the high risk of infection.
You can find your medication here
➔ Medication for bad breath and bad breathOutlook & forecast
The prognosis for oral inflammation is usually good. The stomatitis heals quickly with appropriate treatment. The disease usually subsides within one to two weeks. Follow-up complaints are not to be expected. The prognosis improves if professional teeth cleaning takes place after the treatment and oral hygiene is carried out particularly carefully from now on.
The prognosis is worse with chronic inflammation of the oral mucosa. Patients have to take medication for a long time, exposing themselves to the risk of serious side effects. In addition, the disease itself is a greater burden, as many foods and drinks are not allowed to be consumed. This can have a negative impact on the patient's wellbeing and quality of life.
If the symptoms do not subside, there may be a chronic illness. A comprehensive examination and treatment in a specialist clinic provides information about the causes and allows targeted treatment. In the case of stomatitis, side effects such as severe pain, bleeding or infections in the mouth and throat can sometimes occur, which must be treated. Life expectancy is not restricted by an inflammation of the oral mucosa.
prevention
One can Inflammation of the oral mucosa not effective prevention because the herpes virus that causes it is too contagious. So far there are no vaccinations. The only thing that can be done is to ensure that the rot is not passed on to those affected who are symptomatic of the disease. This is achieved by keeping the person affected by oral mucosal inflammation away from other people, especially children.
Aftercare
In most cases, patients with inflammation of the oral mucosa have very few and limited follow-up measures available. This disease must first and foremost be treated very quickly and, above all, very early, so that there are no other complications and symptoms in the further course.
As a rule, self-healing cannot occur, so that those affected are always dependent on a medical examination and treatment. In general, a very high standard of hygiene should be observed to prevent re-inflammation of the oral mucosa. The person concerned should also clean the mouth with a mouthwash. The symptoms themselves can be relieved relatively easily with the help of medication.
The person affected should ensure that they are taken regularly and that the dosage is correct in order to limit the symptoms. Parents have to control the intake, especially with children. Patients should ideally keep bed rest and not come into contact with other people so as not to infect other people. As a rule, no further follow-up measures are necessary. The oral mucosal inflammation does not reduce the life expectancy of the person affected.
You can do that yourself
Oral mucosal inflammations are usually associated with other diseases, the most common triggers being herpes viruses. Since herpes pathogens are highly contagious, one of the most important self-help measures is to prevent the infection from spreading.
Anyone suffering from oral mucosal inflammation should strictly ensure that they do not share glasses, cups, plates or other dishes or cutlery. Such utensils should best be cleaned in the dishwasher at at least 60 degrees Celsius. In order to avoid secondary infections, great importance is also attached to proper oral hygiene. The teeth, gums and tongue should be gently cleaned with a soft brush after each meal. A disinfecting, pain-relieving mouthwash can also be helpful.
If the inflammation of the mucous membranes is accompanied by severe pain, over-the-counter painkillers can be taken from the pharmacy. If severe discomfort occurs when eating and drinking, it often happens that the patients drink too little and become dehydrated. Those affected should therefore make sure that they at least drink enough fluids despite the pain. Deficiency symptoms due to low food intake can be prevented by taking dietary supplements. In this situation, multivitamin preparations also support the immune system, which is usually already under attack.
If possible, patients should allow themselves a few days of bed rest. This is particularly indicated if the oral mucosal inflammation is accompanied by a cold or another flu-like infection.