The Rh intolerance, colloquial too Blood group intolerance primarily affects pregnant women and their unborn children in their second pregnancy. The rhesus factor in the mother's blood does not match that of the unborn child in the case of rhesus intolerance, which can lead to significant health complications for the baby. During the regular check-ups during pregnancy, the gynecologist checks the risk for the mother and the baby on the basis of the maternal blood count and with the help of ultrasound examinations. As a precautionary measure, treatment against a possibly existing rhesus intolerance can be initiated.
What is rhesus intolerance?

Rhesus intolerance (Morbus haemolyticus) can arise in two ways: in the first child through contact with the mother's blood, in the second through the fact that the maternal immune system recognizes certain blood group characteristics or Thesus factors in the child's blood as incompatible during pregnancy.
© zanna26 - stock.adobe.com
As Rh intolerance is an intolerance of the blood types of a pregnant woman and her unborn child, which relates to the Rh factor. This can be either positive or negative.
A rhesus intolerance, which is dangerous for the unborn child, only occurs in a woman's second pregnancy. The prerequisite for Rhesus intolerance is that the mother carries the Rhesus factor negative (Rh negative) in her blood. The unborn baby and its father, on the other hand, tested positive for rhesus.
The rhesus factor of around 15 to 20 percent of Europeans is negative, while all others are rhesus positive. Due to the different Rh factors of mother and unborn child, the woman's immune system shows a reaction to the baby's red blood cells in the second pregnancy, which is known as Rh intolerance.
causes
To a Rh intolerance in the second pregnancy it occurs when there is blood contact between the rhesus negative mother and the rhesus positive child during the birth of the first baby.
In this constellation, the father must be rhesus positive. As a result of this blood contact, antibodies against the positive Rh factor of the child develop in the mother's blood, which can lead to significant health problems in the baby.
If a pregnant woman has already suffered a miscarriage or received a blood transfusion, caution should be exercised against Rhesus intolerance during the first pregnancy as antibodies can already be formed.
In these cases, rhesus negative women are treated prophylactically against rhesus intolerance during their first pregnancy.
Symptoms, ailments & signs
Rhesus intolerance (Morbus haemolyticus) can arise in two ways: in the first child through contact with the mother's blood, in the second through the fact that the maternal immune system recognizes certain blood group characteristics or Thesus factors in the child's blood as incompatible during pregnancy. The symptoms are the same in both cases.
One of the main signs of rhesus intolerance is anemia. This is indicated by signs such as noticeably pale skin or a lack of oxygen in the child's organism. The cause is the low number of red blood cells. The red blood cells are the units that take in oxygen and can carry it on.
Organs such as the liver or spleen can enlarge due to increased blood formation. The latter seeks to compensate for the anemia. The increasing breakdown of blood cells can lead to increased release of bilirubin into the blood of the newborn. This can be seen in the classic symptoms of jaundice in newborns.
Medical treatment must start at this stage at the latest. This is because the continued rise in bilirubin can lead to bilirubin deposits in the child's brain. Severe anemia can lead to permanent symptoms such as childhood developmental blockages or hearing problems.
An often fatal rhesus intolerance, hydrops fetalis, is indicated by water retention in the child's body. These symptoms often end fatally before birth.
Diagnosis & course
A Rh intolerance is determined by an analysis of the blood type and Rhesus factor in the maternal blood at the beginning of a woman's pregnancy. This examination is part of the usual prenatal care that the gynecologist carries out.
In addition, the gynecologist controls the development of the unborn child with the help of ultrasound examinations. In these, he can recognize abnormalities such as edema or hydrops fetalis, which can be traced back to a rhesus intolerance. If a rhesus negative woman has already produced antibodies in the blood through a previous pregnancy, a blood transfusion or a miscarriage, early treatment of the rhesus intolerance is essential.
Otherwise, severe damage to the infant such as anemia, brain damage or water retention can result. With timely treatment, there is little risk of the infant suffering permanent damage due to rhesus intolerance.
Complications
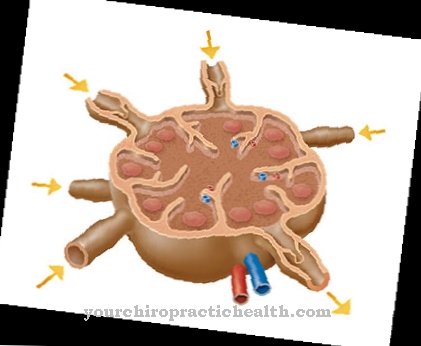
In modern medicine, complications due to rhesus intolerance are rare thanks to comprehensive preventive care and prophylaxis. A rhesus intolerance must be treated, otherwise the child's life is in danger. When antibodies get into the child's bloodstream via the mother, they attach to the child's red blood cells and destroy them. The number of red blood cells is reduced and causes anemia in the child (haemolytic anemia).
The resulting lack of oxygen in the body of the unborn child can lead to developmental disorders and damage to organs. With increasing breakdown of the red blood cells, the bone marrow, liver and spleen try to counteract the loss and thereby swell. This leads to an overload of the liver, the swelling impairs the blood flow and water leaks from the blood into the child's body tissue. This accumulation of fluid is visible on ultrasound. If left untreated, the child can die in the womb.
After birth, there is a risk of oxygen deficiency due to the anemia. In addition, it can lead to excessive jaundice, which must be treated so that the breakdown products do not build up in the brain and cause severe neurological damage. If this severe jaundice is not treated appropriately by experienced doctors, the child's life is in acute danger.
When should you go to the doctor?
The earliest case a doctor will intervene is when a rhesus-negative mother-to-be does not produce antibodies during her second pregnancy. In this case, a rhesus prophylaxis measure between the 28th and 30th week of pregnancy is used to prevent rhesus intolerance.
As part of a medical prophylaxis, the expectant mother in the 28th-30th In the week of pregnancy and within 72 hours of the birth, anti-D immunoglobins or antibodies were injected. The baby's rhesus-positive blood cells, which are in the maternal circulation, are destroyed as a result. With this prophylaxis measure, the unborn child does not suffer any harm, as the antibodies are broken down quickly. It is only ensured that the maternal organism does not produce any antibodies.
If a newborn is intolerant to Rh, it depends on the severity of this phenomenon. In most cases, medical treatment is unavoidable as it leads to anemia and jaundice. In a milder case of rhesus intolerance, phototherapy with blue light may be sufficient. The effect is that the bilirubin molecules can be broken up and excreted. Failure to do so could result in brain damage in the newborn.
In a severe case of rhesus intolerance, it will not go without blood transfusions. In such cases, transfusions may be necessary during pregnancy. Today, thanks to medical advances, something can be done to both survive.
treatment
Treatment of the Rh intolerance takes place during the first pregnancy. In the 28th week of pregnancy, the expectant mother with negative Rhesus factor receives preventive Rhesus factor antibodies, which prevent the development of Rhesus intolerance.
These anti-D immunoglobulins, i.e. the antibodies, are administered again within three days of the Rhesus-positive baby being born. This repeated administration eliminates any risk to the child due to rhesus intolerance in a further pregnancy.
To rule out the risk of rhesus intolerance, an antibody screening test is also carried out in the mother's blood during pregnancy. If abnormalities occur here, a timely response can be made in order to exclude rhesus intolerance and to minimize the risks for the unborn child.
If complications occur, the consequences for the newborn can vary. If the rhesus intolerance is mild, phototherapy or blood transfusion for the newborn baby is usually sufficient. In severe forms such as hydrops fetalis, the newborn baby must be treated in intensive care to ensure survival despite rhesus intolerance.
prevention
To one Rh intolerance As a preventive measure, it is essential to have regular gynecological examinations as a pregnant woman.The mother's blood tests and ultrasound checks on the unborn child can almost completely rule out the risk of rhesus intolerance.
Aftercare
In the case of rhesus intolerance, no special or direct follow-up measures are usually possible, and sometimes these are not even necessary. Those affected should request a diagnosis at an early stage and initiate treatment so that there are no complications or other complaints in the further course of the disease. The sooner the rhesus intolerance is recognized, the better the further course of the disease will usually be.
Therefore, consult a doctor at the first signs and symptoms of the disease. Treatment is usually only necessary after the child is born. Before the birth and during pregnancy, however, further examinations and regular checks by a doctor are very important. The children are dependent on the intake of various drugs.
This significantly alleviates the symptoms and prevents complications. Sometimes the parents are dependent on the support and also on the help of friends and family. This can prevent the development of depression and other psychological upsets. The further course of the Rh intolerance depends heavily on the time of diagnosis, although the life expectancy of the person affected is usually not reduced by the disease.
You can do that yourself
If you have rhesus intolerance, it is essential to seek medical support. The possibilities that doctors have at their disposal are life-saving when the organism is intolerant. Otherwise there is a risk of the premature death of the mother or child. In severe cases and if treatment is refused, the mother and child can die.
The alternative healing methods or home remedies do not work in this area. Since it is a problem and incompatibility of the blood groups, the administration of medication is imperative. Therefore, in the case of an existing pregnancy, cooperation with a doctor should be sought and maintained. Consult a doctor as soon as the first irregularities, malaise or a vague feeling of illness appear. This is the only way to ensure that the necessary measures and health checks are initiated at an early stage.
There are no other approaches that fall into the area of self-help in the case of rhesus intolerance. If the pregnant woman adheres to the treatment options, complications or side effects are hardly to be expected today. Thanks to the medical possibilities, both mother and child can survive today.


.jpg)


.jpg)






.jpg)

.jpg)
.jpg)











.jpg)