A Mycosis fungoides is a rare tumor disease that originates from degenerate T lymphocytes and manifests itself primarily in the skin tissue. The course of the tumor disease is chronic, progressive and poor, whereby the prognosis of mycosis fungoides can be significantly improved by starting therapy early.
What is mycosis fungoides?

© Double Brain - stock.adobe.com
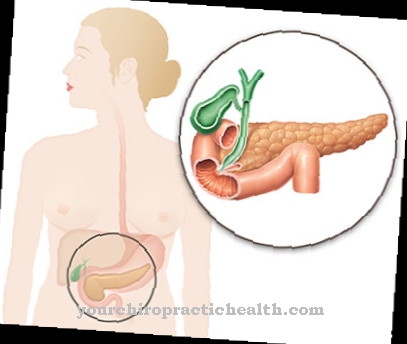
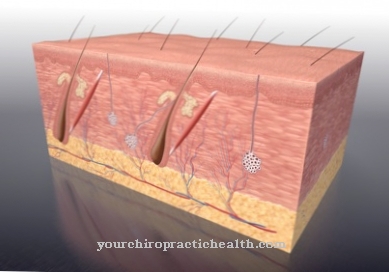
As Mycosis fungoides is a rare, low-grade (less malignant) cutaneous T-cell lymphoma that has a chronic progressive course and originates from malignant T-lymphocytes. The degenerated T lymphocytes attack the skin and cause the skin damage that is characteristic of mycosis fungoides.
Mycosis fungoides is classified as a non-Hodgkin lymphoma (NHL, tumor disease of the lymphatic tissue) and has some special forms that result in a significantly less favorable prognosis. In so-called mycosis fungoides d’emlée, tumors in the skin and mucous membrane (mouth, nose, pharynx) manifest themselves from the start, while in more advanced stages of the disease the internal organs (especially lymph nodes, liver, spleen) can be affected.
In the so-called Sézary syndrome, a greatly increased concentration of degenerate, atypical T lymphocytes can also be detected in the blood (leukemic form of mycosis fungoides).
causes
A Mycosis fungoides is based on one or more degenerate T lymphocytes, which fulfill an important function in the body's own immune system as defense or killer cells.
The degenerated T-lymphocytes attack the skin (cutaneous T-cell lymphoma) and cause the symptoms characteristic of mycosis fungoides such as stubborn, eczema-like skin changes. The triggering factors for this degeneration process could not yet be clarified. A connection between certain viruses (especially the retrovirus HTLV-1) and mycosis fungoides has not yet been proven.
In addition, long-term contact with carcinogenic substances was found in many of those affected who work in the agricultural or metalworking sector. Chronic inflammation, which causes an increased growth of T lymphocytes, is also discussed as a triggering factor for mycosis fungoides.
Symptoms, ailments & signs
Mycosis fungoides can initially be completely symptom-free. The first signs are skin changes that are reminiscent of psoriasis. In addition, painful eczema forms on the skin, which scars over the course of the disease. The skin appears dry and irritated, which can lead to itching and reddening of the skin.
The disease can also cause edema on the skin. These can become infected and in the worst case lead to a bacterial superinfection. If the tumor spreads to healthy tissue, this can lead to irreversible skin damage. Then mental complaints often develop, such as inferiority complexes and social fears.
The mycosis fungoides progresses progressively, so it causes ever greater health problems. If the lymphatic system and the internal organs are involved, cardiovascular complaints, gastrointestinal complaints, hormonal disorders and other health problems arise. This greatly reduces the quality of life.
If the tumor is treated early, the symptoms will subside completely within a few weeks to months. With advanced mycosis fungoides, scars and surgical scars may remain. Early treatment prevents further symptoms and possible long-term effects, whereby the symptoms usually subside a few weeks after the start of treatment.
Diagnosis & course
A Mycosis fungoides is usually diagnosed using a biopsy (tissue removal) from the diseased skin areas. If abscess-like accumulations of lymphoid cells are found in the removed epidermal tissue, mycosis fungoides can be assumed.
The diagnosis is confirmed by a blood analysis. If an increased lymphocyte concentration and / or an increased number of immunoglobulins of class E can be detected, the diagnosis is considered confirmed.
Mycosis fungoides has a very slow course and causes only a few characteristic symptoms at the beginning. In general, the tumor disease has a poor (unfavorable) prognosis and definite healing is extremely rare. If left untreated, the tumor cells of mycosis fungoides spread to the internal organs (liver, spleen) via the blood and lymph systems.
Complications
Since mycosis fungoides is a tumor disease, in some cases it can also spread to other and, above all, healthy tissue and lead to irreversible damage there. For this reason, it is not possible to make a general prediction about the symptoms and the course of the disease for this disease. With early treatment, however, complications and consequential damage can be avoided.
Those affected mainly suffer from discomfort on the skin. The skin is reddened and usually also affected by unpleasant itching. The skin is also very dry and can be flaky. Many patients feel uncomfortable with the symptoms and as a result suffer from inferiority complexes or from reduced self-esteem.
In some cases it also leads to social exclusion and thus to depression and other psychological upsets. Mycosis fungoides can be restricted and treated with various therapies. The success of the treatment depends heavily on the timing and severity of the tumor.
The mycosis fungoides may also limit the patient's life expectancy. Chemotherapy in particular can lead to various complications and side effects that significantly reduce the quality of life of those affected.
When should you go to the doctor?
Symptoms such as itching or reddening of the skin may indicate a tumor that needs to be examined and, if necessary, treated medically. A visit to a doctor is recommended if the symptoms persist for more than a few days or if they rapidly increase in intensity. If the disease is detected early, the prognosis is good. That is why you should speak to your family doctor if you have any initial suspicions. Affected people should also see a dermatologist. Anyone who has already suffered from a tumor is one of the risk patients and should speak to the responsible doctor.
The same applies to people with a weakened immune system or other physical complaints that encourage the growth of a tumor. Medical help is required at the latest when complications such as severe pain or hormone fluctuations are noticed. In addition to the family doctor, an internist or a dermatologist can be visited. In the case of serious illnesses, an orthopedic examination is necessary so that any damage to the bones and joints can be recognized and treated.
Treatment & Therapy
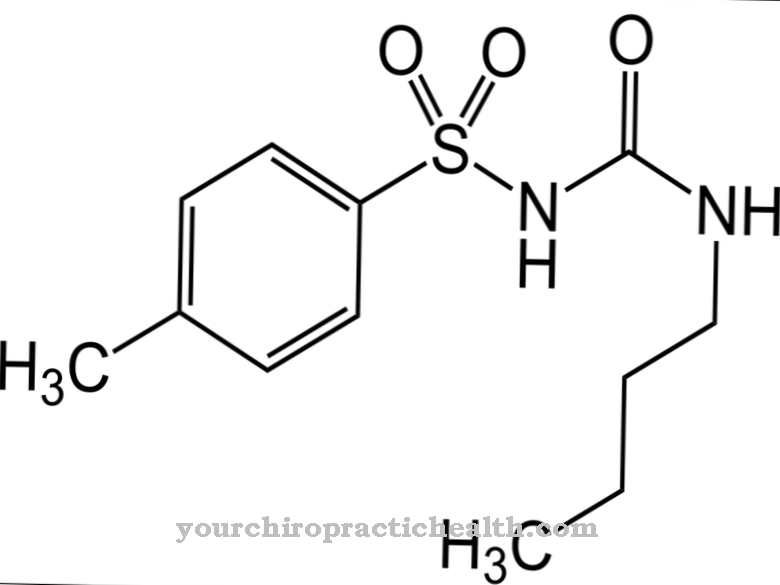
The therapeutic measures depend on one Mycosis fungoides on the current stage of development of the tumor disease. At the beginning of mycosis fungoides (stage I with enlarged lymph nodes and eczema-like, scaly patches), photochemotherapy or PUVA (psoralen plus UV-A) and cortisone ointments are usually used to treat the atypical skin changes.
As part of this therapy, psoralen (photosensitizing substance) is applied locally or orally a few hours before exposure to long-wave UV-A light. In some cases, radiation of the locally limited, atypical skin lesions with X-rays is sufficient at this stage. In the advanced development stage of mycosis fungoides (stage II with plaque and nodule formation up to stage IV with involvement of the internal organs), PUVA therapy is used in combination with immunotherapy with interferon-alpha.
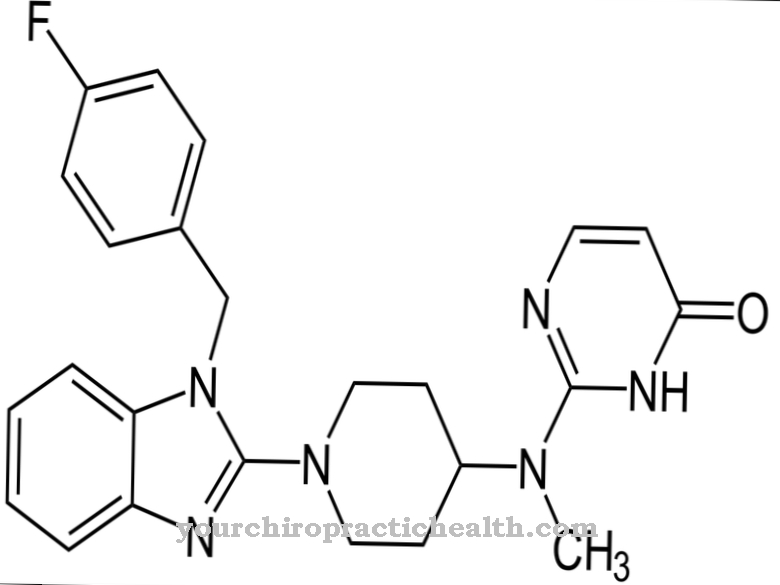
If the lymphatic system and the internal organs are involved, additional chemotherapy and radiation therapy measures are usually indicated in mycosis fungoides. The administered chemotherapeutic agents (especially cytostatic agents) destroy the tumor cells and inhibit cell growth.
Depending on the tolerability and response to the therapy on the part of the person affected by mycosis fungoides, chemotherapy comprises several cycles as well as an individually adapted drug mix (including prednisolone, cyclophosphamide, adriblastine, vincristine).
Outlook & forecast
The prognosis of mycosis fungoides is based on the stage of the disease. Healing is possible in stage I. The condition can persist for many years and cause persistent physical discomfort. In the course of stage II mycosis fungoides, severe complications such as internal organs are affected, which ultimately lead to death. Quality of life and life expectancy are accordingly severely restricted.
The prospect of an improvement in the symptoms is no longer given in stage II. Only chemotherapy can be considered in the case of lymph node and organ involvement in an advanced stage of the disease. However, the treatment also damages healthy tissue and results in complications such as hair loss, gastrointestinal diseases and an increased susceptibility to infection.
Chemotherapy is a great strain and stress for those affected and can leave lasting damage. Stage III mycosis fungoides is usually not treatable. Large parts of the skin are diseased, as a result of which the patients suffer from chronic pain and severe discomfort, which cannot be reliably treated with medication. Stage IV mycosis fungoides has a short life expectancy because large parts of the body are affected.
prevention
Since the causes of the cell degeneration process in a Mycosis fungoides are not clarified, there are no known preventive measures. In general, possible triggers of mycosis fungoides such as carcinogenic substances should be avoided and chronic inflammation treated at an early stage.
Aftercare
In most cases, the person affected with mycosis fungoides has only very limited or very few direct follow-up measures available. The person concerned should therefore consult a doctor very early to prevent further complications and complaints from occurring. The earlier this tumor is recognized and treated, the better the further course of the disease is often.
Therefore, those affected should ideally contact a doctor at the first signs of the disease. Patients often depend on the use of different medications and also on the use of different ointments and creams. The doctor's instructions should be followed, with regular intake and use as well as the prescribed dosage.
If anything is unclear or if there are severe side effects, those affected should always consult a doctor with mycosis fungoides. Many of those affected are also dependent on psychological help during treatment, whereby the support of their own family can have a very positive effect on the further course of the disease. In some cases, mycosis fungoides also reduces the patient's life expectancy.
You can do that yourself
In the case of mycosis fungoides, the possible self-help measures depend on the stage of the tumor disease. In the first stage, the symptoms can be alleviated with cortisone ointments and comparable preparations. Combined with an individual diet and moderate exercise, the growth of the tumors can be slowed down and the healing process supported.
In the advanced stages, mycosis fungoides must be treated in hospital. The therapy can be supported by the patient with various preparations from naturopathy and homeopathy. The most important self-measure, however, is to keep a complaint diary and record any symptoms and complaints in it. Based on this information, the medication can be optimally adjusted. If chemotherapy is carried out, the patient has to take it easy and at the same time change his diet.
The therapy is a great burden for the body and the psyche, which is why extensive preparatory measures must be taken. Together with the patient, the doctor will take appropriate steps to reduce the symptoms and make the therapy as pleasant as possible. Therapeutic advice is also useful. In conversation with a psychologist, the illness can be dealt with and dealing with it easier.

.jpg)

.jpg)






.jpg)
.jpg)
.jpg)







.jpg)