From the olfactory mucosa to the olfactory bulb, the Olfactory nerve as the first cranial nerve, the olfactory information via unmarked nerve fibers. Specific diseases of the olfactory nerve include anosmia and hyposmia. They can also occur as a result of a skull base fracture.
What is the olfactory nerve?
Odors reach the brain from the olfactory mucous membrane via the olfactory nerve. The olfactory nerve forms both the first cranial nerve of a total of twelve and the first link in the olfactory tract, which maps the course of olfactory information transmission.
Disturbances in this area lead accordingly to a pathological deterioration of the olfactory sense (hyposmia) or to complete failure (anosmia). Since the olfactory nerve does not consist of brain stem neurons but is composed of the axons of the olfactory cells, some sources in the specialist literature do not consider it to be a cranial nerve in the narrower sense. For traditional reasons, however, medicine still counts the olfactory nerve among the cranial nerves today; the same applies to the optic nerve or optic nerve, which has similar properties.
Anatomy & structure
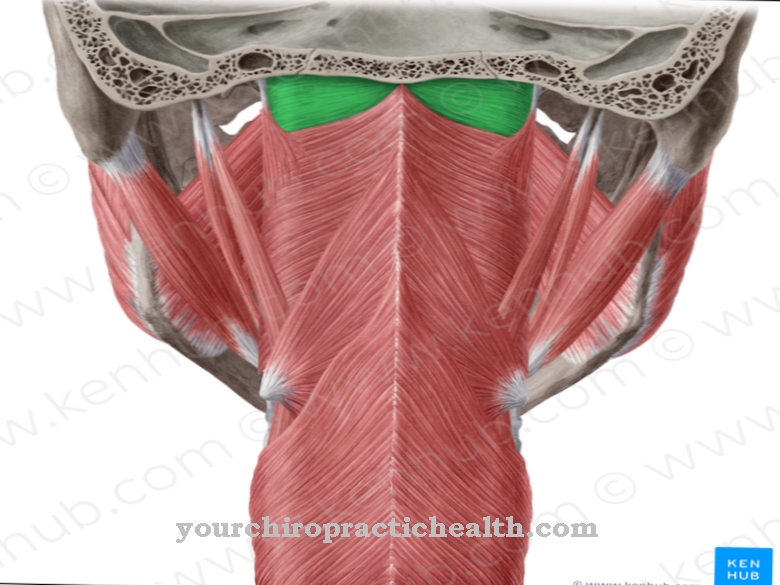
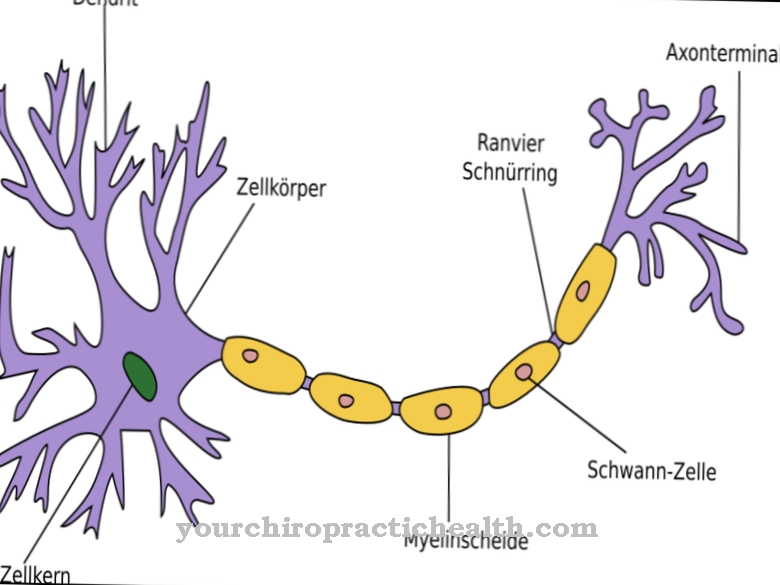
The olfactory nerve consists of fibers, which anatomy also knows as olfactory threads or fila olfactoria. They are the nerve fibers of the cells that sit in the olfactory mucosa and react there to olfactory stimuli. They occur exclusively in the olfactory region. From there the olfactory nerve runs over the lamina cribrosa to the olfactory bulb in the brain. Overall, the olfactory nerve consists of 20-25 bundles, which in turn are made up of the individual nerve fibers (axons).
The nerve fibers that unite to form the olfactory nerve, unlike other neurons, are medullary because they do not have a myelin sheath. The myelin sheath is made up of Schwann cells and electrically isolates the axons. This increases the speed of information forwarding. Conversely, for the olfactory nerve (which lacks this insulating layer), this means that its signals move more slowly than the impulses of other nerves. The olfactory nerve is the shortest of the cranial nerves.
Function & tasks
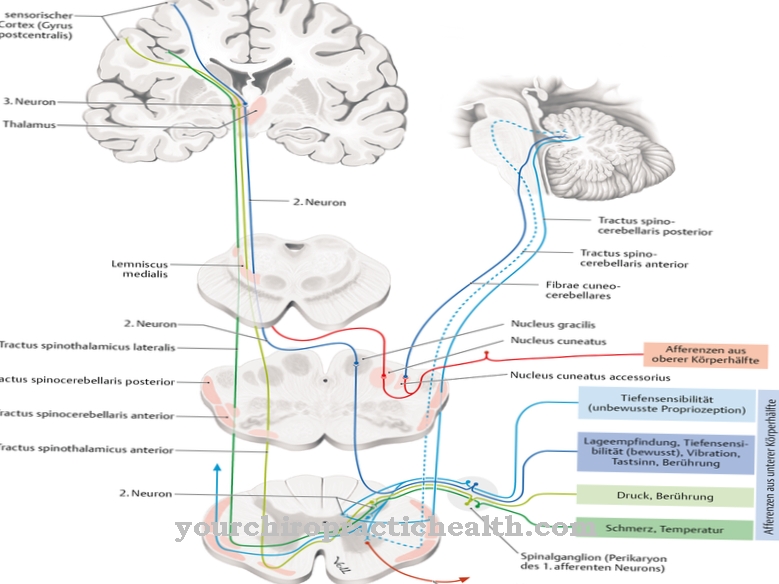
The task of the olfactory nerve is to transmit olfactory information. Although humans are not among the most odor-sensitive living beings in the animal kingdom, their olfactory mucous membrane has over 30 million olfactory cells that are distributed over 10 cm2. The olfactory cell has sensitive receptors on its surface. Irritation changes the properties of the cell membrane and the biochemical balance of the sensory cells shifts. As a result, it comes to depolarization: The electrical voltage changes and can now continue via the nerve fibers.
The long extensions of the cells reach into the olfactory bulb (Bulbus olfactorius), which is already in the brain. No synapse or connection is necessary; the forwarding of the electrical signal is therefore particularly efficient. In the olfactory bulb are the pyramidal mitral cells, which together form the olfactory tract. The signal finally reached the olfactory center of the brain via this second neuron, which neurosciences refer to as the primary olfactory cortex or trigonum olfactorium. This is where the first processing takes place in the central nervous system before the brain uses the olfactory information in higher areas.
You can find your medication here
➔ Medicines for colds and nasal congestionDiseases
Two clinical pictures specifically affect the olfactory nerve: anosmia and hyposmia. The latter describes a decrease in the ability to smell, while people suffering from anosmia lose their sense of smell completely. In the case of functional anosmia, those affected theoretically still have a residual olfactory ability, but its practical significance no longer exists.
Partial anosmia is a special form of olfactory loss, which leads to the loss of olfactory ability for certain fragrances without other olfactory perceptions having to be impaired. Medicine counts these clinical pictures among the quantitative olfactory disorders; there are many causes. Neurodegenerative diseases such as Parkinson's, Alzheimer's or multiple sclerosis come into consideration as reasons for hyposmia and anosmia as well as traumatic effects. The base of the skull fracture is one of the most common traumatic causes of quantitative olfactory disorders, especially in the case of a frontal fracture.
Biochemical causes include zinc deficiency, as well as drugs such as ACE inhibitors, antihistamines, and certain antidepressants. In addition, chlorine and benzene gases can damage the olfactory system, as can infections with viruses, inflammations, tumors and swellings. Congenital anosmia does not necessarily have to be due to an abnormal development or a lesion of the olfactory nerve, but can also affect other links in the transmission of information; However, the cause is mostly in the olfactory tract, which also includes the olfactory nerve. A special form of congenital anosmia manifests itself in the context of Kallmann syndrome; In this case, the olfactory disorder is associated with an underactive ovary or testicle and can thus prevent or delay pubertal development.
In addition, a movement disorder of the hands (synkinesia) and a lack of attachment for teeth and / or cerebral bars are possible, other disorders are also possible. The Kallmann syndrome is due to a mutation in the genetic make-up and is hereditary. Regardless of their cause, anosmia and hyposmia can cause psychological stress; in the case of causes such as neurodegenerative diseases, the psychological symptoms of the respective underlying disease are added, with depressive symptoms being particularly common. Despite intact taste buds and nerves, olfactory disorders also limit the perception of taste, since the two sensory modalities are closely linked and the smell has a decisive influence on the taste of food.



.jpg)


.jpg)


.jpg)




.jpg)