Of the Vagus nerve is the tenth of a total of twelve cranial nerves whose nuclei are located directly in the brain. The vagus nerve makes up the largest part of the parasymphaticus and is connected to almost all internal organs via multiple branches. In addition to its parasympathetic control function of the internal organs via its visceromotor fibers, it also has motor and sensorimotor afferents.
What is the vagus nerve?
The vagus nerve - also simple Vagus called - is the widely ramified Xth cranial nerve, which innervates almost all internal organs. The vagus nerve is also the largest nerve of the parasymphaticus. Its name is derived from the Latin vagus and means something like wandering, unsteady. In its parasympathetic capacity as a supplement and abolition of increased vegetative activity by the sympathetic system, it has general and special visceromotor and viscerosensitive fibers, but also somatosensory and motor afferent and efferent fibers.
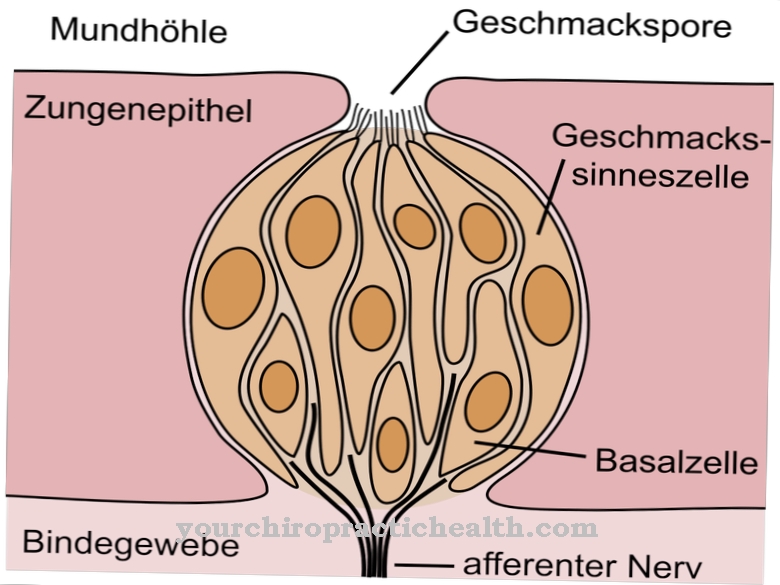
In particular, in addition to its functions in the vegetative area, the vagus nerve is responsible for the conscious motor movements in the pharynx and for some of the taste sensations as well as for touch sensations in the pharynx. The vagus nerve is often referred to in the specialist literature with the IX. and XI. Hinrnerv (tongue-pharynx nerve or leg nerve) combined to form the vagus group. The vagus nerve reaches the lungs, heart, kidneys, liver and the digestive organs via multiple branches and not only controls the parasympathetic vegetative activities, but is also responsible for triggering certain reflexes.
Anatomy & structure
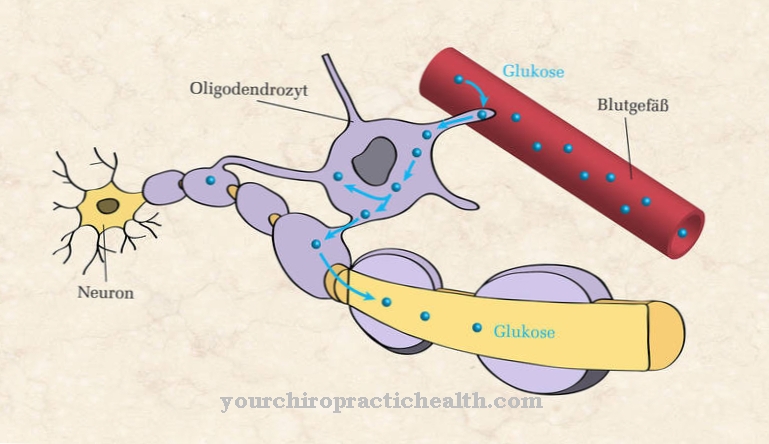
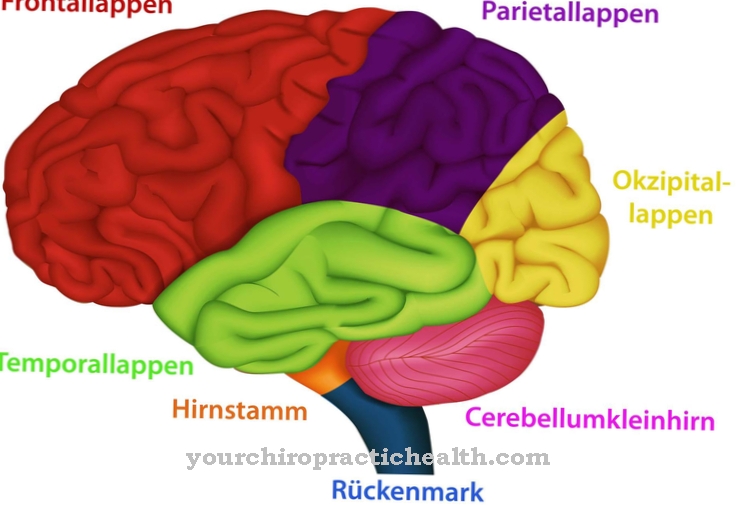
The nerve cell bodies of the parasympathetic neurons of the vagus nerve are located in a core area of the medullary brain (myelencephalon), while the cell nuclei of the motor fibers are located in the nucleus motorius nervi vagi, a region that is also included in the medullary brain. In the area of the medulla oblongate, the elongated spinal cord, the nerve comes to the surface of the brain and leaves the skull through the large opening at the base of the skull (jugular foramen) and passes through two closely spaced ganglia. The cell bodies of the afferent nerve fibers of the vagus nerve ascending from the target organs are located in the ganglia.
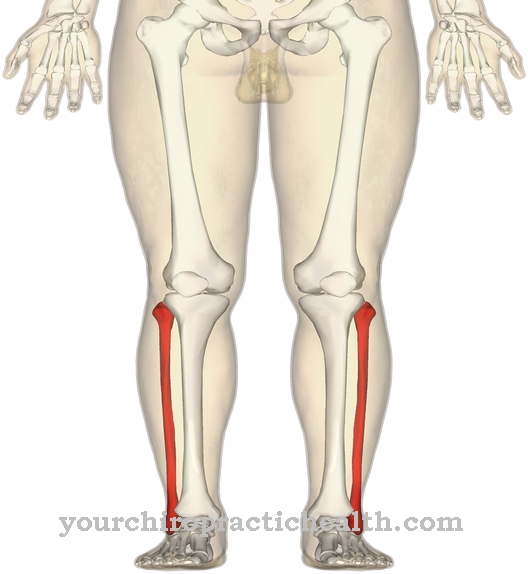
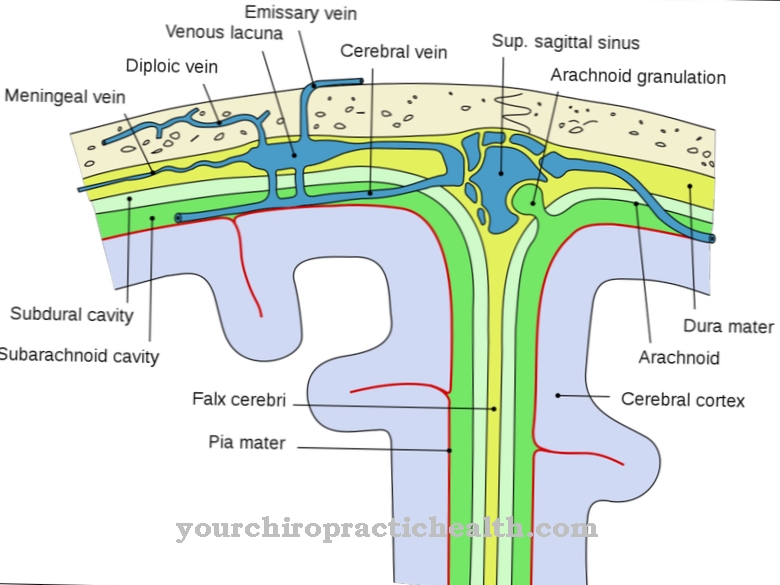
The further course of the nerve and its branches is mostly related to the course of larger arteries or z. B. also ajar against the esophagus. The vagus on the neck runs together with the carotid artery and the large jugular vein in a shared connective tissue sheath, the carotid vagina. The passage through the diaphragm takes place together with the esophagus through the hiatus oesophageus. The ramus meningeus arises from the first branch below the base of the skull and pulls back into the skull through the jugular foramen in order to innervate the meninges (dura mater) of the posterior fossa in a somato-sensitive manner.
Function & tasks
The tasks and functions of the vagus nerve are subdivided according to the affiliation of their efferent or afferent nerve fibers to the vegetative parasympathetic system or to the somato-sensory or motor system of conscious sensory and motor functions. In connection with the parasympathetic control of the innervated organs as an antagonist of the sympathetic control, various protective reflexes are to be understood that can be triggered by activities of the vagus. The most important protective reflex is the vagus reflex. It can be triggered by a blow to the larynx or upper abdomen, by the sight of blood, or by stress, fear or severe pain.
It leads to a widening of the veins with a sudden drop in blood pressure and a slowdown in the heart rate, so that it can lead to dizziness, paleness and impaired consciousness or even fainting. In extreme cases, so-called reflex death or vagus death can occur. In the normal case, the vagus fulfills the task with regard to its parasympathetic functions to return the internal organs to their normal state after a sympathetically increased activity and alertness and to initiate the regeneration phase. This mainly happens at night during the longer rest and sleep phase.
The most important organs on which the vagus and its branches parasympathetic influence are the heart, liver, kidneys, spleen, stomach and most of the intestine including the small intestine and about two-thirds of the large intestine. Outside of the parasympathetic area, the vagus with its motor, afferent fibers is responsible for the conscious motor function in the pharynx and for the transmission of somato-sensory, efferent, feedback from the same area.
Diseases
In principle, symptoms can arise that are caused by weak nerve impulses in the vagus nerve or as a result of excessive activity of the nerve. Functional impairments due to impaired conductivity of the vagus in both the afferent and the efferent direction can have mechanical-physical causes or a disease of the nerve itself or other neurological problems.
Vagotonia or parasympatheticotonia is an excessively strong activity of the parasympathetic nerve or the vagus nerve as the main representative of the parasympathetic system in relation to the sympathetic nerve. Symptoms include low blood pressure (hypotension), slow heart rate, cold hands, cold feet, and narrow pupils. The distinction between vagotonia as the normal state of well-trained people and pathological vagotonia is fluid and difficult to decide in individual cases. A well-known form of vagus disorder is superior laryngeal neuralgia. The superior laryngeal nerve is a side branch of the vagus nerve which, due to inflammation, causes pain when swallowing, coughing and speaking.
Special drugs are used for therapy and, if the effect is too weak, supplemented by neural therapy with a locally effective anesthetic. A possible therapy for treating epilepsy is vagus nerve stimulation (VNS), in which the vagus nerve is electrically stimulated at certain intervals. A distinction is made between the invasive and the transcutaneous VNS. With invasive VNS, the stimulation device is connected to a branch of the vagus via an electrode in the chest area and sends automatic stimulation pulses. The transcutaneous VNS makes use of the fact that a sensitive side branch of the vagus supplies part of the auricle and is located there directly under the skin and can absorb stimuli transcutaneously.







.jpg)

.jpg)
.jpg)











.jpg)