In the Renal replacement therapy the kidney function of a patient with renal insufficiency is partially or totally replaced. The procedures range from various dialysis methods to kidney transplants. A transplant is necessary because dialysis is permanently associated with severe damage to the blood circulation.
What is kidney replacement therapy?

Renal replacement therapy corresponds to the medical treatment route for complete renal insufficiency. Renal replacement therapy treatments partially or completely replace the kidney function. Therapeutically, there are several individual procedures with this goal: Hemodialysis, peritoneal dialysis and kidney transplantation are the best known of them.
Therapy methods such as hemodialysis and peritoneal dialysis are also summarized under the term renal replacement method. Renal replacement procedures are used for both temporary and permanent partial or total loss of kidney functions. Processes such as ultrafiltration also fall into this methodological group. As the transplantation of a donor kidney into an organ recipient, kidney transplantation is the most rigorous kidney replacement procedure.
Function, effect & goals
The kidneys perform detoxifying functions. Without this detoxification, humans cannot survive in the long term. Total kidney failure is therefore life-threatening. To save the patient's life, kidney replacement therapy with detoxifying properties must be given. Which method is used is decided on a case-by-case basis. For example, a donor kidney transplant is the only treatment option other than dialysis for patients with end-stage renal disease.
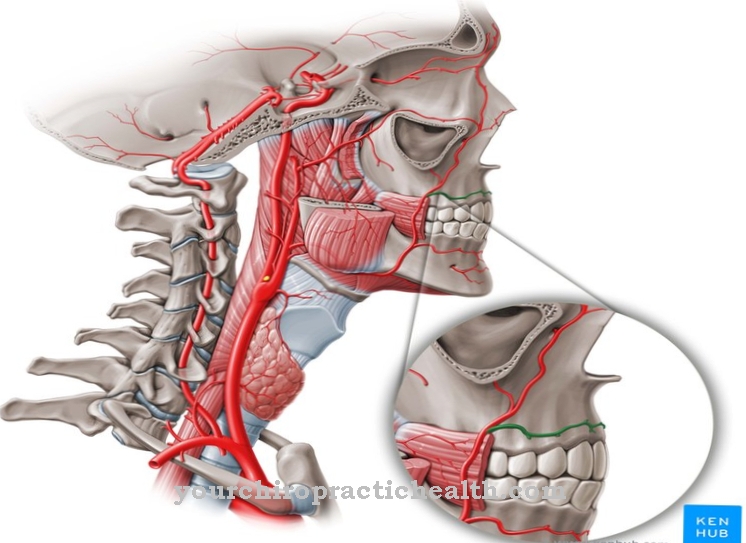
After a living donation or a post-mortem donation, a new kidney is transplanted into the patient in an allogeneic, heterotopic or substitutive transplantation. The blood group and immunological constitution of the donor and recipient must largely match so that a transplant can take place. Usually the kidney is not transplanted in the actual position of the kidneys, but in the pelvic area. Your own kidneys usually stay in the body and the new kidney supports them in their work from now on. For this purpose, the blood vessels of the donor kidney are sutured to the pelvic vessels. The ureter of the graft is connected directly to the bladder. As a rule, the new kidney will start working during the transplant.
To avoid rejection by the immune system, the patient is usually given immunosuppressive drugs. However, some patients are generally not eligible as transplant recipients. This is especially true for patients in whom a certain disease triggers the kidney disease and will allow it to recur after a transplant. In such cases, dialysis procedures are indicated as renal replacement therapy. The same applies to patients for whom no suitable donor kidney can be found in the near future. In renal replacement therapy peritoneal dialysis, the peritoneum, i.e. the peritoneum, serves as the dialysis membrane. Dialysate is let into the abdominal cavity during treatment. The peritoneum is used as a membrane to flush out substances that are subject to excretion.
Access to the peritoneum is made possible by a catheter system. This system is guided into the abdominal cavity by means of subcutaneous tunneling. In hemodialysis, on the other hand, a dialyzer filters the substances that have to be eliminated from the blood. To ensure the blood flow into the dialyzer, the nephrologist puts a so-called dialysis shunt on the patient. These three methods of renal replacement therapy are by no means the only ones. In the area of dialysis procedures, for example, SLEDD and ultrafilitration are also part of the kidney replacement procedures, which are regarded as a type of special dialysis. However, no dialysis can permanently replace a kidney. As soon as the kidneys fail completely, a transplant is indicated in the long term.
Risks, side effects & dangers
The different kidney replacement therapies are associated with different risks and side effects. For example, abdominal pain is common with peritoneal dialysis. Fever is also a common side effect. If the work is not performed sterile, infections and fungi can be brought in via the catheter system. Wound infections at the point of entry of the catheter also occur.
Compared to hemodialysis, peritoneal dialysis releases more proteins, but less creatinine and urea. In the long run, any dialysis can damage blood vessels, joints, or even the heart. Dialysis procedures are a great physical and psychological burden for the patient and require strict guidance on certain dietary rules. For example, foods that contain potassium must be avoided as this increases the risk of heart disease. Since dialysis flushes vital vitamins from the body, dialysis patients also have to take nutritional supplements. They usually perceive their quality of life to be limited.
Since many dialysis procedures take place once a day, they are even no longer free to plan their everyday lives. Kidney transplants limit the quality of life significantly less in the long term. This therapeutic approach is also the only kidney replacement therapy that can be used effectively over the long term. It improves the quality of life and the general state of health of patients, but like dialysis it is associated with risks. In addition to the general risks of surgery and anesthesia, there is always a risk of rejection with a kidney transplant. This risk is enormously stressful for the patient psychologically. Rejection may still occur even if the body appears to have accepted the kidney immediately after the operation.
Although immunosuppressants generally reduce the rate of rejection, rejection in a transplant is never entirely impossible. Inflammatory immune reactions are also at risk. Nevertheless, from a certain stage onwards, transplantation is the only possible kidney replacement therapy.







.jpg)