A Oculomotor palsy refers to the paralysis of the so-called oculomotor nerve (3rd cranial nerve). Oculomotor paresis is a cranial nerve disorder and is an extremely rare disease. It occurs with approximately the same frequency in both sexes.
What is oculomotor palsy?

© designua - stock.adobe.com
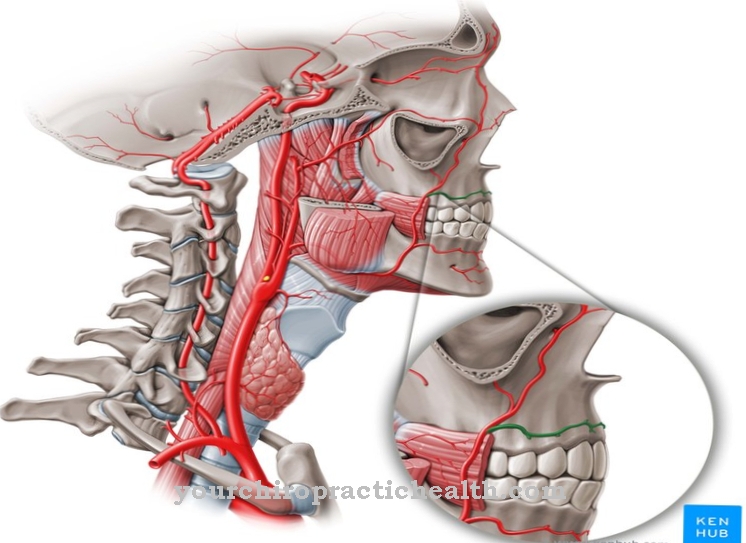
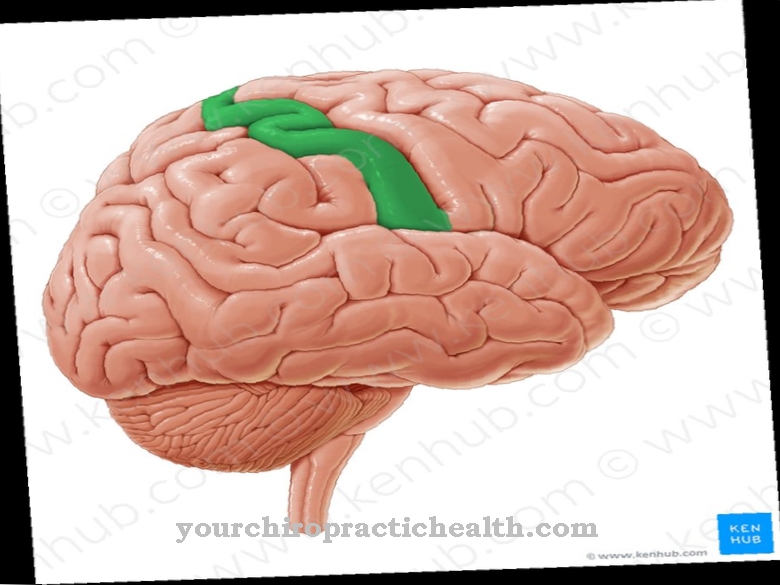
The oculomotor nerve innervates a large proportion of the external eye muscles via motor fibers and two thirds of the internal eye muscles. For this reason, a disorder of the oculomotor nerve can, depending on its location and extent, cause very complex impairments in eye mobility and perception.
Depending on which muscles the paresis affects, there is an internal and an external one Oculomotor palsy distinguished. This can appear in the form of a unilateral or bilateral paralysis. It can also be located centrally in the core area or located on the periphery. In addition, the oculomotor paresis can occur only partially or completely and in combination with other paralysis of the eye muscles.
causes
The causes of damage to the oculomotor nerve can be very different. In the case of impairments in the core area (medical nucleus nervi oculomotorii), supranuclear disorders must be taken into account in many cases. These include, for example, tumors in the brain stem, circulatory disorders or aneurysms. Damage that is located in the peripheral course can also be caused by compression mechanisms, space-occupying processes or trauma.
This can be the case with the so-called Clivuskanten syndrome. Oculomotor paresis is often an accompanying symptom in the context of a more pronounced disease complex, such as Nothnagel syndrome, Weber syndrome or Benedict syndrome. In addition, in a number of cases, combination disorders occur with simultaneous involvement of other cranial nerves, which also contribute to the innervation of the external eye muscles. This can apply to the so-called cavernous sinus syndrome.
Combined paralysis of the oculomotor nerve and the abducens nerve can be diagnosed with some certainty. On the other hand, a simultaneous disturbance of the trochlear nerve is less easy to determine and therefore more easily overlooked. Oculomotor paresis also occurs with increased frequency in connection with diabetes mellitus.
Symptoms, ailments & signs
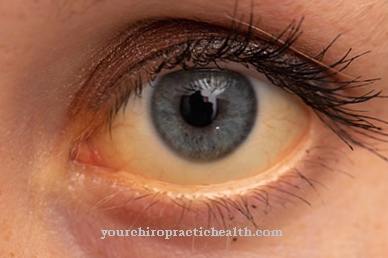
The most important symptoms of oculomotor paresis include a wide, light-rigid pupil or so-called absolute pupil rigidity. The ability to optically close up (accommodation of the eye) is also only possible to a limited extent. In the presence of an isolated, internal oculomotor paralysis in which the external eye muscles are not involved, the disease is referred to as ophthalmoplegia interna.
In addition, a distinction is made between two forms of oculomotor paresis, each of which differs from one another in terms of their symptoms. The symptoms in the presence of a complete oculomotor paresis are characterized by the total failure of the corresponding eye muscles. They manifest themselves in a disorder of accommodation and the pupil reaction and a mydriasis (widening of the pupil) and ptosis (drooping of the eyelid). In addition, the affected eye is directed outwards and downwards.
The second form of oculomotor palsy is partial oculomotor nerve paresis. This is again differentiated into an internal and an external paresis. As part of the external paresis, paralysis of the oculomotor nerve occurs, which results in a disruption of mobility in the external muscles of the eye. Here, too, the eye is directed downwards and outwards. The internal paresis of the oculomotor nerve manifests itself in a disruption of accommodation and the occurrence of mydriasis. In this case, however, there is no malalignment of the eyes.
Diagnosis & course of disease
Many different diagnostic tools can be used in diagnosing paralysis of the eye muscles. As part of the diagnosis of oculomotor paresis, checking the line of sight is of great importance. This procedure uses simple measures to check the extent to which the patient is able to follow the eight directions of gaze.
The patient is usually asked to follow the doctor's moving fingers with his eyes and at the same time to keep his head motionless. Instead of the finger, the test can also be carried out with a pen or stick. If one of the viewing directions is not possible, conclusions can be drawn about the affected impaired eye muscle and the respective disturbed nerve.
Complications
The oculomotor paresis affects the paired oculomotor nerve, which is also referred to as the third cranial nerve or the eye movement nerve. Because the nerve supplies several outer and two inner eye muscles as well as the eyelid lifter, a failure or partial failure of the motor fibers leads to complex loss of movement of the eyes and eyelids.
Complications to be expected with or without treatment largely depend on the causal factors and on whether the oculomotor palsy occurs in isolation or in conjunction with other diseases. Oculomotor paresis usually occurs due to compression of the oculomotor nerve. Such compressions can be caused by space-occupying processes such as growing tumors or aneurysms that press on the nerve.
Another causative factor can be an insufficient supply of the nerve because the supplying vessels are arteriosclerotically narrowed or the blood flow is disturbed for other reasons. An exact diagnosis of the factors that caused the paresis or partial paresis of the nerve is of elementary importance in order to provide targeted treatment as early as possible.
If left untreated, the prognosis in the case of a malignant tumor or aneurysm in one of the supplying vessels can lead to immediately life-threatening complications. Even after treatment that was able to eliminate the cause, a prognosis of the chances of recovery or of further complications can hardly be made. The extent to which the eye movement nerve has already been irreversibly damaged cannot be predicted with certainty beforehand.
When should you go to the doctor?
Any abnormalities in the eyes and eyesight must be examined by a doctor. If the person concerned cannot clearly see objects or people in the immediate vicinity, action is required. A doctor must be consulted so that various tests can be used to investigate the cause. Rigidity of the pupil is characteristic of oculomotor palsy and must be investigated.
If the eye muscles cannot be moved and coordinated sufficiently and according to their own will, a visit to the doctor is necessary. A doctor must be consulted in the event of visual changes in the eye, a drooping eyelid or an eye malposition.
If the discomfort increases the risk of accidents or falls, everyday life must be restructured. There are complications that should be avoided through increased security. A doctor should be consulted so that the person concerned is adequately informed about his state of health and the corresponding consequences.
If there are psychological problems in addition to the physical limitations, a doctor is also required. If you experience persistent stress, fear, anxiety or uncertainty, you should see a doctor. If there are changes in behavior or a depressed mood, the person concerned needs help. If existing complaints increase in intensity or if further irregularities occur, medical support should be sought in order to improve the quality of life.
Treatment & Therapy
Since it is a neurological disorder, therapy must be carried out by a neurologist after the cause has been clarified. In many cases of oculomotor paresis, which are triggered by tumors, trauma or aneurysms, the prognosis is unfavorable. Malnervations often occur during the regeneration process. On the other hand, the chances of recovery from circulatory disorders are more positive as the cause.
If the situation has not improved noticeably after about a year, a squint operation may be necessary. The aim of this surgical procedure is to shift the field of simple vision into the original position without having to adopt forced head postures and possibly to enlarge it. Depending on the findings, the affected muscles are primarily operated on. In the event that the paresis is only minor, the adaptation of prismatic lenses can improve the patient's situation.
You can find your medication here
➔ Medicines for eye infectionsOutlook & forecast
With internal or external oculomotor palsy, the prognosis depends to a large extent on what the underlying condition is. Oculomotor palsy can lead to complex visual impairments. The damage is unilateral or bilateral to the eye muscles. Such damage is triggered by compression pressure from extensive brain tumors. Diabetes mellitus, trauma, aneurysms, or other diseases that affect the brain and eye muscles can also be triggers.
The prognosis depends on the extent and extent of the oculomotor paresis. With a one-sided effect, the prospects are better than with a bilateral effect. The decisive factor, however, is whether and how successfully the underlying disease can be treated. The prognosis is poor if the trigger is to be found in trauma, a tumor or an aneurysm. This can lead to nerve damage with far-reaching consequences for vision.
The outlook is better if the trigger is a treatable circulatory disorder. If the strabismus associated with oculomotor paresis has not improved enough after a year, it can be corrected surgically. Simple vision is improved so that no head posture arises. The field of vision should be expanded again. In the case of more pronounced paresis, the prognosis can be improved by fitting prism glasses.
prevention
There are no direct measures to prevent oculomotor paresis. It is all the more important to consult a doctor immediately in the event of symptoms and disorders of the visual system. This is particularly essential because the oculomotor paresis can also indicate serious diseases such as brain tumors.
Aftercare
In most cases of oculomotor paresis, the patient has only a few and limited follow-up measures available. The person affected should first and foremost consult a doctor at an early stage so that there are no further complications or other complaints that could reduce the patient's quality of life.
Therefore, a doctor should be contacted as soon as the first symptoms and signs of the disease appear in order to prevent further symptoms from occurring. Most of those affected are dependent on a surgical procedure, which can permanently alleviate the symptoms. After such an operation, exertion, stressful or physical activities should be avoided.
In many cases, the support and help of one's own family is necessary in order to prevent depression or mental disorders. The further course of the oculomotor paresis is strongly dependent on the time of diagnosis, so that a general course can usually not be given. The life expectancy of the person affected may also be reduced by this disease.
You can do that yourself
Oculomotor paresis can impair the ability to react in certain everyday situations, so patients should see a doctor in good time. If the eye can no longer see in all directions, this may be due to an insufficient supply of the nerve concerned.
A healthy lifestyle helps against arteriosclerotic constriction or other circulatory disorders. However, it takes a while before you can see any improvement. If those affected have problems recognizing their immediate surroundings correctly, the risk of accidents increases significantly. Patients should therefore learn to assess their visual performance correctly and rather to be a little careful. Certain adjustments in everyday life can prevent falls and other accidents. The doctor also helps to clarify sensible safety measures. In this way, the physical impairments do not automatically lead to emotional problems.
If the stress increases due to oculomotor palsy, it may result in a depressive mood or an inner restlessness. If circulatory disorders are the cause of the disease, the chances of recovery are looking pretty good. It becomes more difficult if the oculomotor paresis is caused by a tumor, aneurysm or trauma. It is all the more important that patients follow all recommendations of the medical professional.


.jpg)
.jpg)

.jpg)