A Ovarian inflammation, also called andexitis or Oophoritis is a disease of the ovaries. Oophoritis can be triggered by a bacterial infection. In rare cases, however, oophoritis is caused by viruses.
What is oophoritis?

© timonina - stock.adobe.com
The Oophoritis In very few cases actually only affects the ovaries - The fallopian tubes are also inflamed, so that - in addition to oophoritis - there is also an inflammation of the fallopian tubes.
Especially women who are of childbearing age are at risk.
About two-thirds of all women who are already in their teens have had ovarian inflammation before. Bacteria, mainly chlamydia, transmitted through unprotected sex, can cause oophoritis.
causes
Different viruses and bacteria can be responsible for causing women to develop oophoritis. As a rule, chlamydia is the trigger; the doctor often also finds streptococci. Sometimes enterococci can also cause oophoritis. One third of all cases are gonococci, which are responsible for inflammation of the ovaries.
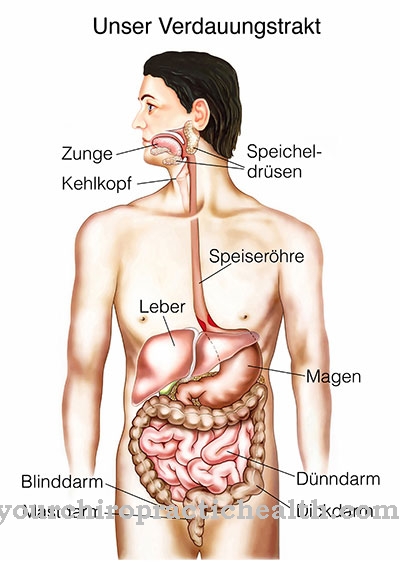
In the context of oophoritis, the doctor speaks of an ascending or descending inflammation. The rising inflammation, which so to speak "rises from the vagina", is triggered by unprotected sexual intercourse and is one of the most common causes of oophoritis. The descending inflammation is triggered by inflamed organs (such as appendicitis), although this form of the disease occurs only in the rarest of cases.
The doctor speaks of haematogenic inflammation even more rarely. The germs - triggered by a virus flu or mumps - reach the ovaries directly through the blood.
Symptoms, ailments & signs
Women who have oophoritis mainly complain of pain in the lower abdomen. In addition to pelvic pain, fever or potential defensive tension can also occur. Sometimes the patient complains of nausea and vomiting.
If those symptoms occur, a medical evaluation should be obtained immediately. However, there are also disease courses that do not bring any symptoms. While many women complain of flu-like symptoms, other patients only visit the doctor because they have bleeding outside of their periods.
Diagnosis & course of disease
Before a pelvic exam is performed, a comprehensive medical history begins. The doctor does a vaginal palpation examination; signs of oophoritis can also be detected by means of an ultrasound examination. For example, if the ovaries or fallopian tubes are already enlarged.
The ultrasound examination should also provide information about whether there are already cysts or whether there is fluid in the abdominal cavity. Pressure pain in the vaginal area or in the area of the uterus is also classic. If the patient reacts to the pressure, this can also be a first sign that oophoritis is present. A blood test provides information about which pathogen triggered the oophoritis or it is also possible to determine the pathogen by means of a vaginal smear and the following examination using a microscope.
The germ is detected in the laboratory - with the help of special cultures. If the patient complains of very severe pain or if the doctor finds that the ovaries are enormously enlarged, an operation often has to be planned. Using laparoscopy (abdominal cavity mirroring), the doctor has an insight into other organs and can sometimes check whether these or even the peritoneum are already affected.
If the disease is treated too late or not at all, a chronic course can result. This means that the woman has to struggle with inflammation again and again, which then leads to the formation of scars, so that fertility sometimes also suffers. Women who have had three ovarian infections have a 50 percent chance of being infertile.
Complications
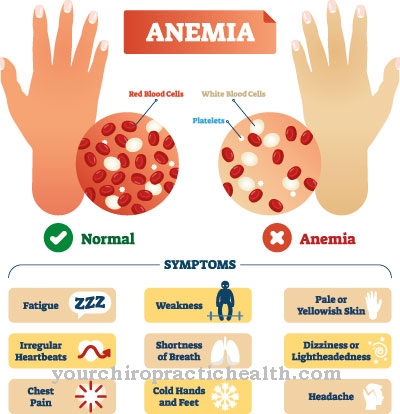
First and foremost, oophoritis is very painful in the abdomen and stomach. This pain has a very negative effect on the quality of life of the person concerned and can also lead to considerable restrictions in everyday life. Furthermore, the patients lose their appetite due to the persistent abdominal pain and suffer from weight loss or various deficiency symptoms.
Oophoritis can also lead to fever, vomiting and nausea, so that the patient's resilience is significantly reduced. In women, this can also lead to increased vaginal bleeding, which can continue to be associated with mood swings. As a rule, oophoritis does not heal itself, so treatment by a doctor is always necessary.
Treatment of oophoritis is usually done with the help of antibiotics and leads to a positive course of the disease relatively quickly. There are no particular complications for those affected. However, if left untreated, oophoritis can lead to appendicitis. The life expectancy of the patient is usually not changed by this disease.
When should you go to the doctor?
Women and girls who suffer from ailments in the lower abdomen that are not related to menstruation should consult a doctor. If pain persists or increases in intensity, a doctor is needed. A feeling of tension in the ovaries or uterus, malaise or a feeling of illness should be examined and treated. If you experience flu-like symptoms such as vomiting, nausea or internal weakness, the cause must be clarified. Fever and a decrease in exercise capacity should be examined and treated by a doctor.
If bleeding occurs outside of the cycle, this is considered a warning signal for the organism. A visit to the doctor is required for a diagnosis to be made. Bleeding when using the toilet, loss of libido and discomfort during sexual intercourse should be discussed with a doctor. If changes in behavior occur, increased tiredness is noticed or if the person concerned complains of insomnia, a doctor should be consulted.
Swelling in the lower abdomen, a decrease in physical activity, and mood swings can all result from oophoritis. A visit to a doctor is advisable so that the restrictions in everyday life do not spread any further. Action is required in the event of deficiency symptoms, exhaustion or a loss of weight. Since no self-healing is to be expected, medical care must be initiated.
Therapy & Treatment
It is important that oophoritis is treated relatively early. This is the only way to prevent possible long-term effects, such as infertility. As a rule, the oophoritis is treated with antibiotics; the antibiotics have to be taken for around 14 days. If the course of the disease is very severe, the treatment can no longer be carried out on an outpatient basis, so that the patient is admitted to the hospital as an inpatient.
Care is taken that - if there is evidence of which pathogen was the cause of the oophoritis - immediate drug treatment takes place. If, for example, bacteria such as chlamydia are involved in the oophoritis, not only the patient but also the sexual partner must subsequently be treated. In addition, anti-inflammatory drugs are used - even for outpatient treatments for oophoritis; Sometimes pain relievers can also be administered.
After the acute phase is over, patients can also take hip baths, fango packs or short-wave heat therapy. Sometimes the “pill” can even be used to “immobilize” the ovary. In addition to conservative methods, the doctor can also opt for an operation. Especially if previous treatments have not been successful or if complications (appendicitis or peritonitis) are already present.
Even in the case of very severe scarring, the doctor can - together with the patient - agree that the fallopian tubes or ovaries are removed so that a symptom-free life can be led.
Outlook & forecast
There are hardly any diseases like acute inflammation of the fallopian tube and ovaries in a woman, so there are so many synonyms. A distinction must be made between an acute and a chronic form of oophoritis. In general, both diseases are summarized as bacterial inflammation of the female appendages. These are dealt with under the medical umbrella term "adnexitis".
The prognosis for acute oophoritis naturally differs from that of the chronic form of oophoritis. Acute adnexitis is common in young and sexually very active women. In most cases, the prognosis is favorable because the acute adnexitis can heal without consequences. The important prerequisite for this, however, is that the infection is diagnosed at an early stage and not spread. After adequate treatment, acute oophoritis can heal without any consequences.
The prognosis is slightly worse if there are complications in the acute stage. Examples of this are an abscess on the fallopian tubes and ovaries, or peritonitis. In both cases, the fallopian tubes can become permanently glued as a result of the associated symptoms being carried over. As a consequence, the women affected would have to reckon with permanent infertility.
If the gynecologist does not receive treatment at the first symptoms of oophoritis, the inflammation of the female appendages can become chronic.
prevention
Ovarian inflammation can be prevented if both partners opt for protected sexual intercourse (using a condom). Ultimately, chlamydia, or other bacteria that are transmitted through sexual activity, are the main triggers.
Aftercare
In most cases, the person affected with oophoritis has only limited direct follow-up measures available. For this reason, the person affected must consult a doctor as soon as the first symptoms and signs of the disease appear, so that further complications or complaints can be prevented. In the worst case, if left untreated, the affected person will be completely infertile, which cannot be reversed.
Therefore, early diagnosis is the main focus of this disease. In most cases, oophoritis is treated by taking various medications. It is always important to ensure that the dosage is correct and that the medication is taken regularly in order to alleviate the symptoms. If antibiotics are used to treat the disease, they should not be taken with alcohol.
Regular checks and examinations by a doctor are also very important after treatment in order to detect and treat damage to the internal organs at an early stage. Typically, oophoritis does not reduce life expectancy if detected and treated early. Further follow-up measures are not necessary and are usually not available to the person concerned.
You can do that yourself
Women who have ovarian inflammation should first adhere to the guidelines of the gynecologist. The pain relievers and anti-inflammatories must be taken according to the doctor's instructions so that the healing proceeds optimally.
A whole range of natural remedies such as yarrow, horsetail or oat straw can be taken to accompany this. Homeopathic preparations such as Belladonna or Aconitum have anti-inflammatory effects and may also be used in consultation with the doctor. Affected women should also dress warmly and wear sturdy shoes. After intercourse, which should take place with a condom in the first few weeks after diagnosis, careful personal hygiene is required. Chronically ill people should permanently ensure good intimate hygiene.
If you experience any unusual symptoms or complaints during or after the treatment, it is advisable to see a doctor. The medical professional can monitor the progress and adjust treatment if necessary. He can also call in a homeopath and other medical professionals if there is a serious underlying disease or if the oophoritis does not subside within a few days or weeks. The patients should also take sufficient care of themselves and avoid contact with the cold.










.jpg)

.jpg)
.jpg)











.jpg)