As orthostatic dysregulation is a regulation disorder of blood pressure. It occurs when the person concerned assumes an upright posture.
What is orthostatic dysregulation?

© 9nong - stock.adobe.com
The orthostatic dysregulation is also called in medicine Orthostasis Syndrome or orthostatic hypotension known. What is meant is a regulation disorder of the blood pressure when the person changes to an upright body position.
The term orthostasis comes from the Greek and means "standing upright". The orthostatic dysregulation is counted among the forms of arterial arterial hypotension. There is a malfunction of the orthostasis reaction, which in healthy people ensures that the cardiovascular system works properly even in an upright position.
However, orthostatic hypotension results in symptoms such as palpitations, feelings of weakness, dizziness and nausea if the person adopts an upright posture. If the person concerned sits down or lies down again, the symptoms quickly subside.
Medicine divides the regulatory disorder into three forms:
- sympathetic orthostatic hypotension
- the asympathetic orthostatic hypotension
- postural orthostatic tachycardia syndrome.
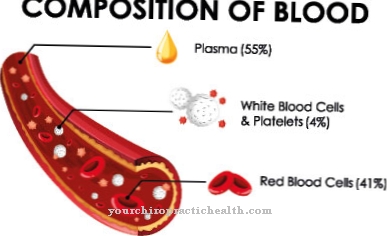
causes
While the term hypotension refers to low blood pressure, orthostatic hypotension refers to an abrupt drop in blood pressure after standing up. During this process, blood drains from the head towards the feet. In response to this process, the heartbeat drops faster and the blood vessels contract, causing the blood pressure to rise rapidly.
The organism can bring the blood back to the head in a short time. However, if this reaction sets in too slowly, it briefly causes insufficient blood flow towards the brain, which makes the person concerned feel drowsy. Orthostatic dysregulation is not a life-threatening disorder, but it can sometimes lead to loss of consciousness and even to a fall that is accompanied by an injury.
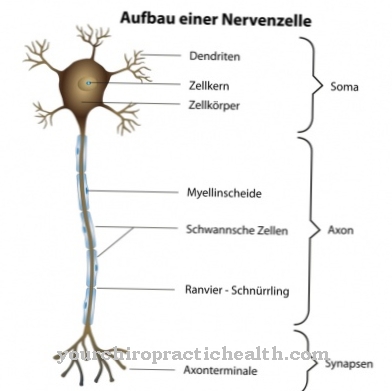
It is not uncommon for an increased age to be responsible for orthostatic dysregulation. Over the years, the body partially loses its ability to respond to orthostasis. But certain diseases are also considered a risk factor for orthostasis syndrome. These include primarily diabetes mellitus and diseases that affect the nerves that are important for blood pressure regulation.
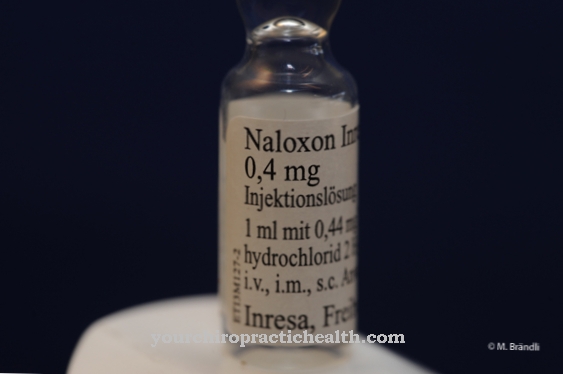
Another possible cause of orthostatic dysregulation is the use of certain medications. These are medicines that work against high blood pressure and dilate blood vessels. In addition to blood pressure drugs, there are also diuretics, cytostatics, drugs against Parkinson's disease, and hypnotics.
But tranquilizers, tricyclic antidepressants, opiates, psychotropic drugs, insulin, muscle relaxants as well as alcohol and drugs such as marijuana can also trigger an orthostasis syndrome. Other possible causes are heart and blood vessel diseases such as heart failure or pericarditis.
Narrowing of the aorta or disorders of the heartbeat, infections, an underactive thyroid, malfunction of the anterior pituitary and adrenal cortex, permanent lack of exercise, prolonged bed rest and a lack of fluids.
Symptoms, ailments & signs
The orthostatic dysregulation is characterized by unspecific symptoms. As a rule, they show up after a sudden change in position of the body, which particularly affects getting up after lying down. If the person concerned stands for a longer period of time, the symptoms can worsen.
General symptoms are a feeling of coldness, nausea, paleness, sweating and inner restlessness. In addition, there are frequent palpitations, a feeling of oppression, dizziness, headache, drowsiness, insecurity when walking and standing, ringing in the ears, eye flickering and a feeling of emptiness in the head.
Because of the discomfort, the patient is forced to sit down or lie down again. In this case, the symptoms usually go away quickly. In some cases, however, a brief fainting is possible, with the risk of a serious fall and associated injuries.
Diagnosis & course of disease
Suspicion of orthostatic dysregulation usually arises from the patient's medical history. To confirm the diagnosis, the attending physician usually performs a tilt table examination or a Schellong test. In the Schellong test, the patient remains on an examination table for five to ten minutes while their blood pressure and pulse are measured.
Then he should get up quickly and stand for five to ten minutes. Pulse and blood pressure are also checked during this period. In the tilt table test, the doctor straps the patient onto a table that can be tilted. After a rest period of twenty minutes, he tilts the table and uses it to straighten the patient.
After being in a standing position for twenty minutes, the table is tilted back and the process repeated. In most cases, orthostatic dysregulation takes a positive course. The symptoms improve in around 80 percent of all patients.
Complications
In most cases, this disease does not lead to any particular complications and, as a rule, does not result in a life-threatening condition. The symptoms and complaints can vary in severity in different patients. As a rule, most people with this disease suffer from paleness and nausea. Headaches and blurred vision occur after changing positions.
Flickering eyes or ringing in the ears can also occur. Walking creates uncertainty and makes those affected appear dazed and confused. The symptoms usually disappear relatively quickly when the patient lies down or sits down. There are no particular complications. However, in severe cases it can lead to unconsciousness in the patient, which may result in injuries.
Treatment of the disease is only necessary in severe cases. This is done with the help of medication and does not lead to further complications. If another underlying disease is responsible for these symptoms, it must be treated first. As a rule, the life expectancy of the person affected is not restricted due to illness.
When should you go to the doctor?
People who experience discomfort after a sudden or rapid change in body position should consult a doctor. If the skin appears pale, feels unwell or nauseated immediately after the exercise, there is cause for concern. Consult a doctor in the event of flickering eyes, dizziness or loss of balance so that there are no sequelae or other problems. Ringing in the ears, headache or a feeling of emptiness should be examined. If there are disturbances in the heart rhythm, a racing heart develops or a loud palpitation occurs, a doctor is needed.
If you feel light-headed after getting up or bending over, you need to clarify the symptoms. A brief loss of consciousness should be reported to a doctor immediately. If possible, the rescue service should be alerted so that the health status of the person concerned is stabilized as quickly as possible. A feeling of coldness, unsteady gait or an increased risk of accident should be brought to a doctor.
If fears develop, a withdrawal behavior or movements are almost completely avoided, the person concerned needs help. In the event of an increase in the complaints or new symptoms, a visit to a doctor is strongly recommended. Often the existing discomfort increases as soon as the person concerned has stood for a certain time and then changes the body position.
Treatment & Therapy
As far as possible, orthostatic dysregulation should be treated without the use of medication. Only in severe cases is the patient given alpha adrenoceptor agonists. In order to counteract hypotension, which usually occurs in the morning hours, it is recommended that you do circulatory exercises when you stand up.
The venous return flow can be stimulated by activating the lower leg muscles while lying down. Before the person concerned gets up, they can sit for two minutes beforehand. A cool environment is also helpful, as the cold also increases the venous return flow. A strong cup of coffee can often help.
Outlook & forecast
The prognosis for orthostatic dysregulation varies. Sympathetic orthostatic hypotension has a positive prognosis. They are easy to treat. In contrast, the asympathetic form of this disease is a serious disease with a poorer prognosis.
In the case of sympathetic orthostatic dysregulation, the person concerned can lead a relatively normal life. However, he should take various measures to keep him healthy. It cannot be ruled out that otherwise deterioration or cardiovascular disease may occur. To what extent an orthostatic dysregulation is merely a nuisance or a harbinger of later cardiovascular diseases, the medical professionals disagree.
In general, blood pressure that is too low is not noticeable because it has a vascular damaging effect. It can cause complaints, but also grant freedom from complaints. Measures that improve the prognosis are helpful. For example, patients should drink more fluids and salt. You should discontinue any medication that promotes orthostatic hypotension. Everyone can do a lot to keep the blood vessels healthy, for example through exercise, Kneipp treatments or brush massages. Those affected with orthostatic dysregulation can do a lot to improve the prognosis. Drug therapies are only necessary if your own measures are insufficient.
The asympathetic variant of orthostatic dysregulation is a chronically progressive form. This is difficult to control with therapeutic measures.
prevention
In order to prevent problems caused by orthostatic dysregulation, it is recommended to get up slowly and not too quickly. It also makes sense to sleep with your upper body elevated.
Aftercare
Orthostatic dysregulation is a clinical picture that often depends on the patient's behavior. Follow-up care is therefore prevention at the same time, so that the disorder occurs as rarely as possible in those affected. There is a whole range of measures that are used in aftercare and can be discussed in advance with the treating doctor, for example the family doctor.
Movement is an important factor in stabilizing the circulation in the long term. Here, individual aftercare for all aspects of orthostatic dysregulation offers two efficient components: On the one hand, it is important to keep moving briefly during the day to activate the circulation, for example to get up from the PC at your desk and do a few gymnastic exercises .
Furthermore, a consistently carried out athletic training is important. Strength training and fitness classes are just as possible as swimming or playing sports. The only important thing is regular circulatory activation. Drinking behavior is also important as part of the follow-up care for orthostatic dysregulation. Drinking too little can lead to dehydration, which can lead to circulatory problems.
Water and teas are particularly suitable as regular drinks. On the other hand, alcohol, especially in large quantities, should be avoided. Nicotine can also have adverse effects. During meals, care should be taken not only to burden the organism with lavish portions, but rather to eat light foods more frequently during the day.
You can do that yourself
After medical evaluation and treatment, self-help towards illness is primarily about reducing symptoms and improving quality of life. This increase is possible by paying attention to a few aspects in everyday life.
Since long periods of standing can be problematic, but this cannot always be avoided, compression stockings are a great help in such situations. The pressure on the veins and the muscles in the legs prevents the blood from sinking into the legs as quickly. This reduces the risk of a sudden drop in blood pressure. Furthermore, it is advisable to change position slowly in the case of orthostatic dysregulation. After sleeping, it is advisable to sit for a moment. It is also helpful to get up very slowly after sitting for a long time. This also reduces the risk of blood sinking in the legs and the symptoms of orthostatic dysregulation. Staying in very warm rooms or while bathing is particularly critical.In these cases, care should also be taken to avoid standing for long periods or standing up quickly.
Alternating showers can help to reduce the sensitivity of the nervous system somewhat. This means that when showering, the water temperature should be switched between warm and cold. It is most effective if the phase with cold water lasts about 30 seconds and the leg region is preferred to be showered. Exercise and diet also have a significant impact. Eating too much salt can generally raise blood pressure somewhat, and building good leg muscles will help the body function naturally.

.jpg)

.jpg)













.jpg)