The Osteomyelitis (inflammation of the bone marrow) is a disease of the bone caused by bacteria such as B. Staphylococcus aureus is caused. The focus of inflammation is in the bone marrow and then spreads to the various layers of bone. A distinction is made between endogenous and exogenous osteomyelitis, which can occur in both an acute and a chronic form.
What is osteomyelitis?
.jpg)
© Artemida-psy - stock.adobe.com
The Osteomyelitis is an inflammation of the bone marrow caused by bacteria. For this i. d. R. the bacterium Staphylococcus aureus responsible. Osteomyelitis is divided into endogenous and exogenous. This relates to the development of osteomyelitis.
Endogenous osteomyelitis - also known as hematogenous osteomyelitis - occurs when the bacteria enter the bone marrow via the blood (hematogenous). The bacteria for this originate i. d. Usually from a source of infection inside (endo) the body. Exogenous osteomyelitis occurs as a result of external (exo) injuries. The pathogen enters the bone marrow through the wound.
Acute osteomyelitis is divided into three groups, depending on the age of the person affected. A distinction is made between acute hematogenic infant osteomyelitis, acute hematogenic osteomyelitis in children and acute hematogenic osteomyelitis in adults.
causes
Main cause of a Osteomyelitis are bacteria that cause infection in the bone marrow. In addition to Staphylococcus aureus, salmonella, streptococci and Escherichia coli can be responsible for bone marrow inflammation.
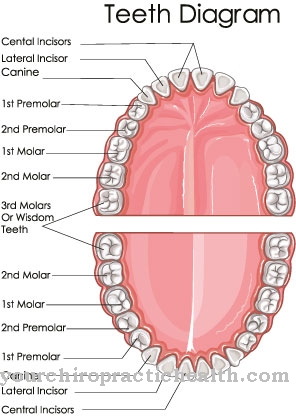
In endogenous osteomyelitis, the bacterium enters the bone marrow via the blood supply. For this, there must be other sources of infection in the body such as B. tonsillitis, inflammation of the sinuses and inflammation of the teeth and mucous membranes. Since the route of infection is via the blood supply, the bacterium can spread over the entire skeleton and lead to severe sepsis.
In exogenous osteomyelitis, the pathogens enter the bone marrow from outside. This can happen as a result of an injury or during an operation. The bacteria mainly spread in the area of the wound, so that the bone marrow inflammation is localized. The risk of exogenous osteomyelitis is increased if e.g. B. diseases such as diabetes mellitus or arteriosclerosis are present and / or the immune system is weakened.
Symptoms, ailments & signs
The acute inflammation of the bone marrow initially leads to a general feeling of illness. The patient feels tired and limp, nausea and fever, sometimes accompanied by chills. After a short time, the area above the inflamed bone marrow begins to hurt. It is tender and swollen.
The skin turns red and feels warm. The bone may pulsate painfully and the limbs lose strength and muscle tension. As the disease progresses, a fistula can develop. Secretions or pus produced by the inflammation must drain away. Therefore it paves a canal through the skin and emerges from the opening of the fistula.
If the infection follows an injury or after an operation, such as after an artificial joint has been inserted, pus can seep out of the unhealed wound. But even if the wound has already closed, inflammation can develop a long time after the procedure, which is known as subacute osteomyelitis.
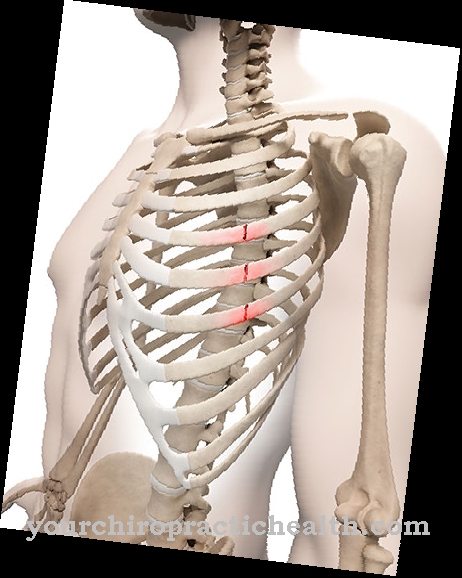
If a joint is involved, this manifests itself in pain with certain movements. Osteomyelitis can affect any bone, but the most common area is the upper arms or knees. If the disease is left untreated, the inflammation can spread throughout the body and cause irreversible damage to the bone marrow.
Diagnosis & course
The diagnosis Osteomyelitis is secured using various diagnostic methods. Since symptoms such as swelling, reddening and restricted mobility can also have other causes, the following blood values are first examined after a thorough anamnesis (medical history).
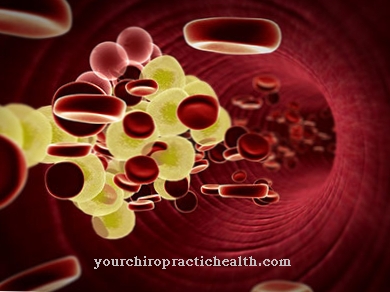
Since osteomyelitis is inflammation, inflammation parameters such as leukocytes (white blood cells), CRP (C-reactive protein) and ESR (sedimentation rate) are increased. The pathogen can be determined with the help of blood cultures.
In addition to laboratory diagnostics, imaging methods such as B. X-rays, ultrasound, magnetic resonance imaging and skeletal scintigraphy are used. However, these examination methods are only used later, as visible changes in the bone become apparent after about two to three weeks at the earliest.
The course of osteomyelitis depends on the type of bone marrow inflammation. Acute endogenous osteomyelitis heals without consequences if it is diagnosed in good time and treated appropriately.
In adults, this form of bone marrow inflammation can often be chronic. As the bones change over the years, they may not respond as well to treatment. As a result, acute attacks occur again and again. Endogenous osteomyelitis takes a chronic course in 10 out of 100 people affected.
In infants or children, endogenous osteomyelitis often takes a severe course and permanent damage occurs. Growth disturbances are the result and the affected part of the body is deformed or shortened. Another consequence can be blood poisoning (sepsis).
In exogenous osteomyelitis, an early diagnosis and adequate treatment have a positive effect on the course and can therefore heal without consequences. However, i. d. Acute osteomyelitis usually turns into a chronic form, which means that the bone changes. Stability and mobility decrease, and the inflammation can spread to nearby joints. In about 6 out of 100 people affected, the part of the body affected is amputated as the osteomyelitis progresses.
Complications
Complications of osteomyelitis usually develop if the disease is not treated in a timely manner. Those affected suffer from a high fever and not infrequently also from exhaustion and permanent fatigue. The inflammation can also spread to the other bone layers. There will also be swelling and redness on the skin.
Due to the osteomyelitis, the patient may also suffer from various mobility restrictions and thus from restrictions in everyday life. In general, the quality of life of the person affected is significantly reduced due to the illness. The joints and bones also hurt and can lead to irritation in the person concerned. If osteomyelitis already occurs in children, this disease can lead to severe disturbances in development and growth.
In the worst case scenario, blood poisoning can also occur, which can be fatal for the patient. The treatment of osteomyelitis is usually relatively uncomplicated and with the help of antibiotics. There are also no complications. The life expectancy of the patient is also no longer affected by successful treatment.
When should you go to the doctor?
If you feel generally ill, unwell or tired, you should consult a doctor. If there is a loss of the usual level of performance or a decrease in resilience, a doctor is required. Flu-like symptoms such as chills, pain or an irregularity in the muscular system should be examined and treated. Symptoms of inflammation, increased body temperature and nausea are signs of a health impairment that should be presented to a doctor. Discoloration of the skin's appearance and a feeling of warmth in the skin are considered worrying.
If the symptoms persist over a long period of time or if they intensify, a doctor is required. Particular caution is required if pus develops. In severe cases, the affected person threatens sepsis and thus a life-threatening condition. A doctor's visit is necessary as soon as the redness spreads to the affected area or sterile wound care cannot be guaranteed. The enlargement of a wound should also be presented to a doctor.
If the everyday requirements can no longer be met or if there are disturbances in the general movement sequences, a visit to a doctor is advisable. Swelling in the immediate vicinity of the bones and sensory disturbances are other signs of an irregularity. A doctor should be consulted as soon as feelings of numbness develop or a tenderness or hypersensitivity to touch occurs.
Treatment & Therapy
The Osteomyelitis is treated with antibiotics. In acute osteomyelitis, the affected part of the body is immobilized using a splint or a plaster cast. If a lot of tissue has also died, this must be surgically removed.
In exogenous osteomyelitis, due to the poor blood flow to the bone, there is limited healing through antibiotics. Because of this, surgical treatment must take place. The affected and destroyed tissue is removed. A so-called spongiosaplasty, a filling of the bone with bone substance from a healthy bone, is also carried out, especially with large-area ablation.
In chronic osteomyelitis, the inflammation is also treated with antibiotics. Surgical treatment is definitely necessary here. Since the tissue is permanently destroyed due to the recurring infections and the inflammation usually spreads uncontrollably, amputation of the affected extremity is medically advisable in good time.
You can find your medication here
➔ Medicines for painOutlook & forecast
Osteomyelitis or inflammation of the bone marrow takes on a chronic course in many cases. The earlier the disease is recognized, the better the prognosis. Osteomyelitis is easier to treat in the early stages. A chronic manifestation and the associated irreversible damage can sometimes be averted.
Both the type and severity of the osteomyelitis influence the prognosis. The age of the sick person, their general health and the group of pathogens are also decisive factors. Acute osteomyelitis has a better chance of a cure than the chronic form. Acute bone marrow inflammation usually heals completely with early treatment. If diagnosed late, it can become chronic. In this case, the prognosis is less favorable, and treatment becomes tedious. There is a risk of circulatory disorders in the bones. The joint can only be moved to a limited extent or not at all. In the case of severe disease, antibiotic drugs can no longer contain the disease. An operation is necessary here. The affected bone tissue is removed during the surgical procedure.
No preventive measures can be taken for osteomyelitis. However, people with stable immune systems were less likely to develop bone marrow inflammation. If a patient has already been treated for osteomyelitis, avoiding overload has a positive effect.
prevention
Preventive measures can be taken for a Osteomyelitis to be carried out conditionally. Since osteomyelitis is caused by bacteria, antibiotics can be administered prophylactically in the event of injuries and surgical interventions.
Further preventive measures must be taken by the hospital / doctor's office. By adhering to the hygiene regulations, the spread of the causative bacteria can be prevented so that the occurrence of osteomyelitis can be reduced to a minimum.
Aftercare
In the case of osteomyelitis, there are usually very few and only limited measures available for direct follow-up care. For this reason, the patient should consult a doctor as early as possible with this disease so that there are no further complications or complaints. The earlier a doctor is consulted, the better the further course of the disease is usually.
Most patients with osteomyelitis are dependent on various medications. If anything is unclear or if you have any questions, you should always consult a doctor first in order to prevent further complications. When taking antibiotics, it should also be noted that they should not be taken together with alcohol.
After treatment for osteomyelitis, regular checkups by a doctor are necessary in order to detect and treat further inflammations or infections early. As a rule, this disease does not reduce the life expectancy of the person affected if it is recognized and treated early. Further follow-up measures are usually not available to the affected person.
You can do that yourself
This disease is mainly caused by different strains of bacteria and patients may need to be treated with antibiotics for months to prevent amputation or blood poisoning. It is therefore important for the patient to support the fight against the pathogens and consistently strengthen the body's immune system.
You should completely avoid alcohol and nicotine, since both are toxins that unnecessarily burden the body. Passive smoking can also be harmful. In return, the patient is advised to eat a light, healthy diet that consists of plenty of fresh fruit, vegetables, sea fish and lean meat. If the patient is able to leave the house, exercise in the fresh air would be advisable, especially walks in the woods. They have been proven to support the healing process.
Since eighty percent of all immune cells are located in the intestine, a supplementary dose of probiotics would also be indicated. Probiotics are mixtures of living microorganisms that are supposed to settle and multiply in the intestine. There they contribute to the maintenance of the immune system.Probiotics are commercially available in the form of yogurt, dietary supplements or medication. The latter contain more microorganisms and are preferable to yogurt.
Another possibility to accelerate the course of treatment is the so-called "hyperbaric oxygen treatment". The patient inhales oxygen in a pressure chamber, which leads to an increased distribution of oxygen in the tissue.


.jpg)






.jpg)

.jpg)
.jpg)











.jpg)