Osteocytes are mature bone cells enclosed by osteoblasts of the bone matrix.
In the case of defects in the bone, osteocytes die due to inadequate supply of nutrients and thus call the bone-degrading osteoclasts on the scene. Pathological osteocytes can be relevant to diseases such as osteoporosis.
What are osteocytes?
The human bone is alive. Immature osteoblasts form what is known as the bone matrix. This network of immature bone cells includes the mature bone cells. They are also known as osteocytes and numerically make up the majority of bone cells.
The osteoblasts are their predecessor. The maturation of the osteoblasts takes place during osteogenesis. This term means the formation of new bone tissue. The body constantly forms new bone tissue and rebuilds the bone structure or adapts it to loads. Demineralization and remineralization are constantly taking place in the bones. Osteoclasts break down old bone substance and are therefore responsible for demineralization.
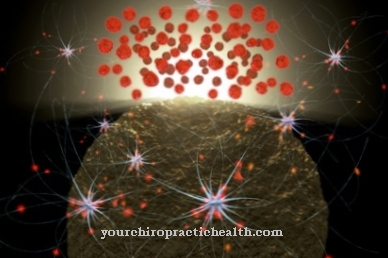
Osteoblasts take over the mineralization. They become trapped in osteogenesis and become mature osteocytes in this cavity system. So-called gap junctions connect the osteocytes with one another. These are cell-to-cell channels that serve to exchange nutrients. The function of the osteocytes has not yet been conclusively clarified. Presumably they are involved in bone loss.
Anatomy & structure
Osteoblasts form what is known as the bone matrix. This is the basic organic substance of the bone that is still unmineralized. Type I collagen fibers and mucopolysaccharides are important components of the bone matrix. They make the bone elastic under pressure.
The embryonic connective tissue is also called mesenchyme. From this, the osteoblasts form in the immediate vicinity of the blood capillaries. These immature bone cells form soft osteoid. This is not yet calcified bone substance. Over time, the osteoblasts enrich the osteoid with the calcium phosphate hydroxylapatite. This deposit hardens and stabilizes the bone. Some osteoblasts are surrounded on all sides by bone matrix. These osteoblasts are the osteocytes. These are mononuclear cells in a cavity system with mineralized bone substance.
The lacunae system of the osteocytes lies between the individual lamellae of the bones. There is a cell body in every lacuna. The cell extensions lie in the fine canicular tubules. The cell extensions connect the osteocytes by gap junctions.
Function & tasks
In human bones, bone formation and degradation takes place permanently. Every seven years the person receives a new skeleton, so to speak. The skeleton adapts to new conditions through the conversion. Stressed bones, for example, become thicker and more resilient over time. Bones that are not moving or that are not under stress are getting thinner and weaker.
Osteoclasts and osteoblasts play a major role in bone metabolism. Osteoblasts build up. Osteoclasts break down bones and prevent the endless growth of bone substance. The breakdown by the osteoclasts is required, for example, in the case of micro-breaks or fractures. In these phenomena, the cells break down defective bone substance. They dissolve the bone through two mechanisms. First, the mineral salts of the bone are removed so that the substance becomes softer. This happens due to a reduced pH value in the cavity between the bone substance and an osteoclast. The low pH value is maintained through active transport of protons.
After the mineral salts have been dissolved out, the osteoclasts release proteolytic enzymes. These enzymes dissolve the collagenous bone matrix and then phagocytize the released collagen fragments. The two breakdown mechanisms of the osteoclasts give rise to Howship lacunae, which are also known as the osteoclasts' feeding track. Each osteoclast can theoretically break down the same amount of bone, which requires almost 100 osteoblasts to build up. The osteoclast activity is hormonally controlled and activated by parathyroid hormone.
Inactivation takes place through calcitonin. Osteocytes are now also assigned a regulatory function. In defective bones, there is little or no nutrient supply via the gap junction. As a result, the osteocytes die in the defective bone matrix. Only when the osteocytes die are the osteoclasts called into action.
Diseases
The bone can be affected by various dysregulations. A decreased activity of the osteoclasts, for example, has just as much disease value as an increased activity of the osteoclasts or a decreased activity of the osteoblasts.
Pathological osteocytes can play a role in dysregulation of osteoclast activity. However, since the exact function of the osteocytes is not yet known, this is a rather speculative relationship. When the activity of the osteoclasts is reduced, the bone proliferates. Bone cancer can develop this way. Decreased osteoclast activity is also related to diseases such as genetic osteoporosis. Increased activity of the osteoclasts breaks down more bone than the osteoblasts can form. This phenomenon plays a role in genetic osteoporosis.
In addition, diseases such as hyperparathyroidism, osteodystrophia deformans, aseptic bone necrosis and rheumatoid arthritis are characterized by this phenomenon. The same is true for periodontitis and osteogenesis imperfecta. The role of osteocytes in the diseases mentioned remains the subject of research. Since dead osteocytes first call the osteoclasts onto the scene, a causal relationship between the structure of the osteocytes and some of the diseases mentioned cannot be ruled out.
Typical & common bone diseases
- osteoporosis
- Bone pain
- Broken bone
- Paget's disease





.jpg)





.jpg)
.jpg)


.jpg)