Of the Peritonsillar abscess is usually a complication of a bacterial infection in the throat and pharynx. The pathological occurrence is most frequently caused by bacteria of the species streptococcus type A. The treatment is equivalent to emptying the abscess with subsequent removal of the tonsils.
What is a peritonsillar abscess?

© stockshoppe - stock.adobe.com
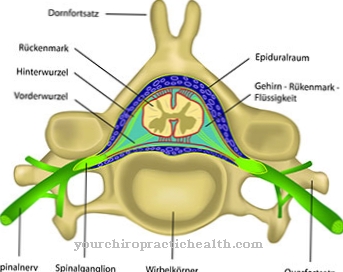
The pharyngeal constrictor muscle is a multi-part muscle that belongs to the throat muscles and is located not far from the tonsils. Abscesses can form in the area between the palatine tonsil and the pharyngeal constrictor muscle. These are encapsulated collections of pus that are located in a preformed tissue cavity. Bacteria are usually involved in the formation of abscesses.
In this case, the pus is a mixture of dead body cells, bacteria and immune cells. When an abscess arises between the tonsils and the pharyngeal constrictor muscle, it is of one Peritonsillar abscess the speech. An untreated peritonsillar abscess is associated with acute danger to life, as the abscess could break into the parapharyngeal space and sink into the mediastinum.
Like every abscess, the peritonsillar abscess also consists of an abscess cavity due to inflammatory meltdown of the tissue and the pus within it. With any abscess there is a risk that it will spread further along crevices and thus increase considerably in size. Abscesses often form fistulas that connect the abscess in the form of a duct system with internal or external body surfaces. The peritonsillar abscess usually corresponds to a bacterial abscess and is therefore not to be understood as a sterile abscess.
causes
Bacterial abscesses develop as a result of a bacterial infection. One such infection is angina lacunaris. This is a form of tonsillitis in which the bacterial deposits extend beyond the structure of the tonsils. Such inflammations are usually the result of an infection with the bacterium streptococcus type A.
The peritonsillar abscess can be a complication of angina lacunaris. The inflammation and with it the bacteria initially spread in the connective tissue between the tonsil and the pharyngeal constrictor muscle, which leads to peritonsillitis. This peritonsillitis eventually results in abscess formation. The abscess does not necessarily have to develop with this etiology.
Even after acute pharyngitis and treatments such as tonsillectomy, a peritonsillar abscess can form if the tonsils have not been completely removed. Since streptococci type A remain the preferred pathogen of the abscess, the peritonsillar abscess is often referred to as an aerobic-anaerobic mixed infection, which is to be expected as a complication of angina lacunaris and, more rarely, of acute pharyngitis.
Symptoms, ailments & signs
The peritonsillar abscess forms as a late consequence of angina lacunaris and accordingly does not occur in the acute phase, but a few days after the inflammation. The patients suffer from unilateral swallowing difficulties, which make it difficult for them to eat. Due to the reduced food intake, those affected are in a rather poor general condition, with their body temperature being infectiously increased.
The language of the patients seems lumpy. Often those affected have a history of stabbing ear pain, also known as otalgia. An excessive saliva production in the sense of a hypersalivation occurs. In some cases, patients can barely open their mouths so that a jaw clamp can be observed. One of the most serious complications of the abscess occurs when it invades the parapharyngeal space.
The abscess, and with it the causative bacteria, sink into the mediastinum and cause mediastinitis that can take on life-threatening proportions. In addition, there is a risk of complications from abscesses spreading to veins in the neck region and finally bacteremia, which can cause sepsis. Like all infections, a peritonsillar abscess can be accompanied by general signs of infection such as chills, fatigue, and loss of appetite.
Diagnosis & course of disease
To diagnose a peritonsillar abscess, the doctor inspects the soft palate, which is usually restricted on one side. Often the anterior part of the palatal arch is reddened or bulges forward. An enlarged, laterally displaced uvula completes the clinical picture.
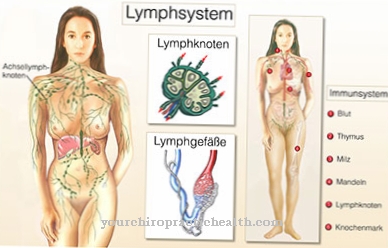
In addition, the lymph nodes are infectiously enlarged and sensitive to touch. The doctor confirms his first suspicions with an ultrasound of the neck area. An x-ray is also used to confirm the diagnosis. If the abscess spreads along the neck fascia, a CT is also done. In the differential diagnosis, the doctor rules out uvular edema. Early diagnosis of the peritonsillar abscess is associated with a favorable prognosis. If the complications mentioned above have already occurred, the prognosis is much less favorable.
Complications
In most cases, this disease can be treated relatively well. Especially with early diagnosis and treatment, there are no particular complications and the disease progresses positively. Patients with this disease primarily suffer from severe difficulty swallowing and a sore throat.
The difficulty swallowing can lead to restrictions in the intake of food and fluids, so that an underweight and possibly also deficiency symptoms can occur. Earache or headache also occur with this disease. Those affected can no longer speak easily, so that there are significant restrictions in the patient's everyday life.
Furthermore, the bacteria can also spread into the blood without treatment, so that in the worst case scenario blood poisoning and thus death of the person concerned can occur. In most cases, the patients also suffer from the symptoms of the flu, so that the person concerned becomes tired and exhausted.
With the help of antibiotics, the symptoms of this disease can be limited. As a rule, complications do not arise and there is no reduction in life expectancy.
When should you go to the doctor?
A peritonsillar abscess must always be treated by a doctor. If no treatment is initiated, this disease can even lead to death of the person concerned. The earlier treatment starts, the higher the chances of a complete cure. A doctor should be consulted if there are severe swallowing difficulties or inflammation in the mouth area, although these symptoms do not go away on their own and are usually more severe than usual. Fever and general symptoms of a Flu coming.
Often language problems also indicate a peritonsillar abscess and should therefore be examined. Many patients can no longer breathe easily and suffer from gasping or hyperventilating. There is also fatigue or chills, with many patients also showing loss of appetite.
The disease is usually diagnosed and treated by a general practitioner or an ENT specialist. The disease usually progresses positively and life expectancy is not reduced.
Treatment & Therapy
Since the peritonsillar abscess can become life-threatening due to complications or a diagnosis that is too late, treatment and thus control of the causative bacteria must be started as soon as possible. Oral or parental penicillin is indicated as soon as the first signs of peritonsillitis appear.
In this way, the formation of the abscess can possibly still be prevented. As an alternative to penicillin administration, drugs such as clindamycin or cefuroxime are available. If a full abscess has already formed, an incision and splay is made. The doctor uses a pair of forceps to do this. A few days after the procedure, it is expanded. This treatment should result in sufficient emptying of the abscess.
If the abscess does not empty sufficiently, an invasive abscess tonsillectomy is performed in the sense of a hot tonsillectomy. A tonsillectomy is indicated even if a satisfactory evacuation has been achieved. If this treatment is not performed around four days after the incision, there is a high risk of recurrence.
You can find your medication here
➔ Medication for tonsillitis & sore throatOutlook & forecast
The tonsil abscess or peritonsillar abscess is a relatively common complication of purulent tonsillitis. Statistically speaking, there are around 40 peritonsillar abscesses per year for every 100,000 tonsillitis cases. Mostly younger adults are affected by an almond abscess.
The dramatic increase in antibiotic resistance in recent times is problematic. As a result, after acute and purulent tonsillitis, painful tonsil abscesses are much more common. The forecast, which is good in itself, can be put into perspective in the future. If antibiotics are no longer effective for an abscess or a purulent tonsillitis, abscesses will probably form more frequently in the future.
The peritonsillar abscess is caused by the spread of bacteria from the ulcerated tonsils to the surrounding tissue. An abscess develops on at least one almond. It is filled with pus and extremely painful. This can lead to a lock in the jaw. The patient develops a fever and severe difficulty swallowing. These can radiate into the ear and also cause the lymph nodes to swell. The prognosis can only be improved if the doctor opens and drains the abscess. Then antibiotics or penicillin are prescribed.
With proper treatment, the prognosis is quite good. However, it does not rule out a repetition of such inflammations and abscess formation. If the tonsils that are prone to inflammation are not surgically removed, there is still a risk of further abscess formation.
prevention
Peritonsillitis can only be prevented to the extent that angina can be prevented. The peritonsillar abscess can in turn be prevented by counteracting incipient peritonsillitis with penicillin.
Aftercare
The peritonsillar abscess requires extensive follow-up care. At the beginning there is severe pain, difficulty swallowing and a fever, all of which severely limit the feeling of wellbeing, but the chances of recovery are usually good. Antibiotic treatment is effective and helps alleviate the symptoms.
Combination therapy, which should quickly resolve the symptoms associated with the abscess, is particularly effective. Life expectancy is usually not limited by a peritonsillar abscess. Only in severe cases can serious complications occur, which can be fatal if the physical condition is poor.
For example, symptoms such as blood poisoning or severe inflammation with a high fever are possible, which under certain circumstances can lead to a circulatory collapse. As part of the aftercare, the complaints must be clarified again in order to rule out complaints and complications. Patients should contact the responsible doctor and discuss the next steps.
If no symptoms are found, no further treatment of the abscess is usually necessary. Aftercare also includes gradually discontinuing the prescribed antibiotics. The doctor should then be consulted again as a final blood test is necessary. If necessary, further imaging procedures must be used.
You can do that yourself
A peritonsillar abscess must be opened and drained by a doctor. At the same time, the tonsils may be removed. The prescribed medication, mostly penicillin, should be taken consistently as directed by a doctor.
Patients need bed rest for the infection to subside. At the same time, they must eat enough, even if swallowing problems and loss of appetite make it difficult to eat. Homemade chicken soup is particularly recommended here, as it is nutritious on the one hand and also compensates for any lack of fluids on the other. Experience has also shown that it can lower a fever. Chicken contains easily digestible protein and the vegetables cooked with it also provide vitamins. Of course, nicotine and alcohol are taboo for patients with a peritonsillar abscess.
As bacteria triggered the disease, intensive oral hygiene is important both during the healing process and for prophylaxis. Even minor damage to the teeth and gums can harbor bacteria and should be treated by a dentist at an early stage. During daily oral hygiene, the teeth are thoroughly brushed at least twice with a toothpaste containing fluoride. The spaces between the teeth should also be cleaned once a day. Dental floss and space brushes are suitable for this.
A healthy diet with lots of fruit, vegetables and whole grain products not only supports the immune system in the fight against further bacterial infections, but also helps to ensure that the oral flora remains intact and can fight off bacteria.










.jpg)

.jpg)
.jpg)











.jpg)