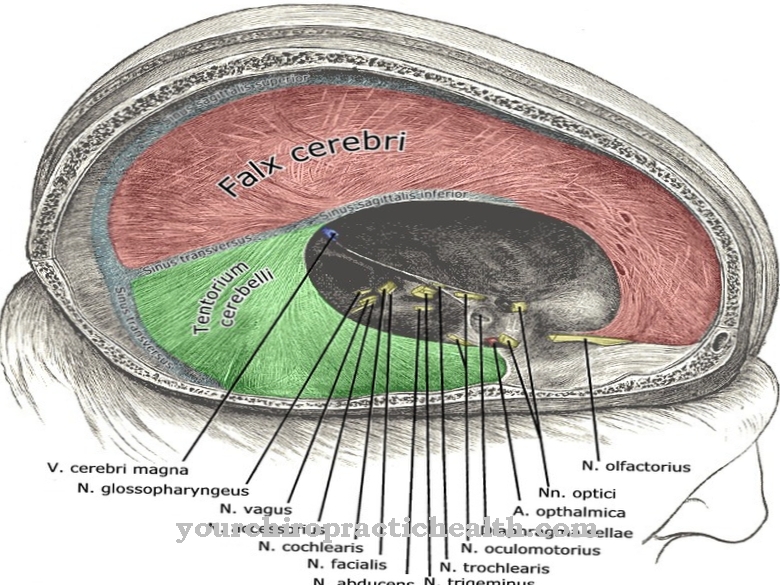
As Plexus anesthesia is called a form of local anesthesia. It is used for surgical interventions or for postoperative pain therapy through a catheter. The anesthetic is injected directly into the area of the plexus and leads to a pain block in the extremity, which is supplied by the plexus.
What is plexus anesthesia?

Plexus anesthesia is a form of anesthesia. By blocking the nerves, the sensation of pain in the relevant extremity is eliminated. This is achieved with a local anesthetic, a so-called local anesthetic. This type of partial anesthesia is indicated for surgical interventions on the upper and lower extremities.
The local anesthetic is injected into the vicinity of nerves, nerve plexuses or the spinal cord.The supply area of the nerve fibers that is to be temporarily anesthetized is decisive for the corresponding nerves. A catheter can be inserted to switch off the sensation of an extremity in the long term. Local anesthetic is continuously added via this catheter and extends the partial anesthesia during ongoing operations or postoperatively for pain relief.
The patient remains awake during partial anesthesia, but can also be given an appropriate drug to calm down or to sleep. This causes what is known as sedation, which puts the patient into a twilight sleep. After the surgery, the patient can be awakened at any time.
Function, effect & goals
In plexus anesthesia, the anesthetist injects an anesthetic into the local nerve plexus or into the nerve trunks. This blocks the sensation and thus also the transmission of pain. The muscles are paralyzed in the area to be operated on.
The place where the anesthetic is injected depends on the region of the body to be operated on. This procedure is often used for the upper extremities. However, it is also suitable for numbing the lower extremities. For the upper extremity, the arm is bent 90 degrees at the shoulder joint and the elbow joint in order to have a clear view of the armpit. The puncture site is found using a so-called nerve stimulator. It is located approximately above the axillary artery. The nerve stimulator is connected to the puncture cannula at the end. If the needle tip of the cannula comes close to the nerve to be anesthetized, this becomes noticeable through muscle contractions in the forearm.
Alternatively, the puncture cannula can also be guided to the corresponding plexus using an ultrasound. When injecting with a nerve stimulator, approximately 40 ml of anesthetic is injected. Long and highly effective anesthetics such as ropivacaine are preferred. It takes about 20-30 minutes for the full effect to take effect. In order to accelerate this, a short and fast acting substance such as prilocaine or mepivacaine can be added.
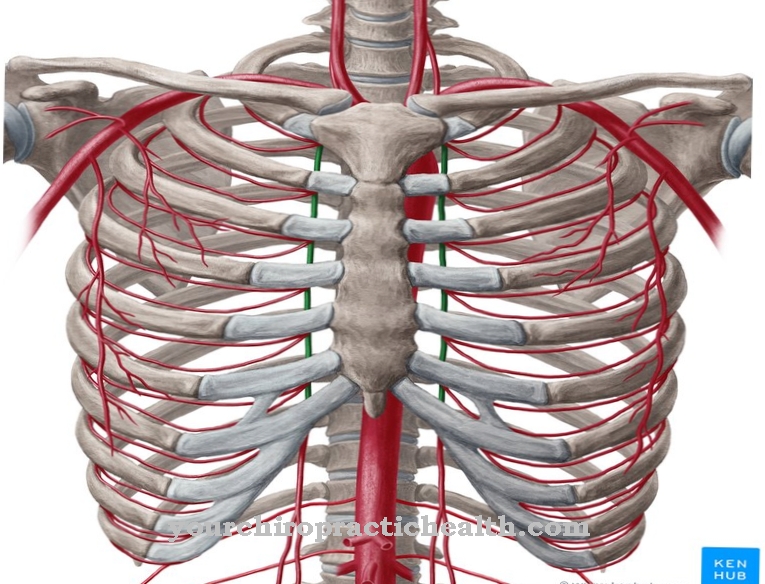
The most common plexus anesthesia is applied to the arm nerve plexus. If a pain block is set in this area, surgical interventions can be carried out in the area of the clavicle, shoulder, upper arm, elbow joint, forearm and hand. A distinction is made between axillary blockade (within the armpit), vertical infraclavicular blockade (below the collarbone) and interscalene blockade (in the area of the neck muscles). The anesthesiologist decides, depending on the medical history and the planned intervention, which pain blockade is indicated and implemented.
If surgery has to be performed on the lower extremity, plexus anesthesia is applied to the lumbosacral plexus. The pain block enables interventions in the area of the thigh, knee joint, tibia and fibula as well as the ankle joint and in the area of the foot.
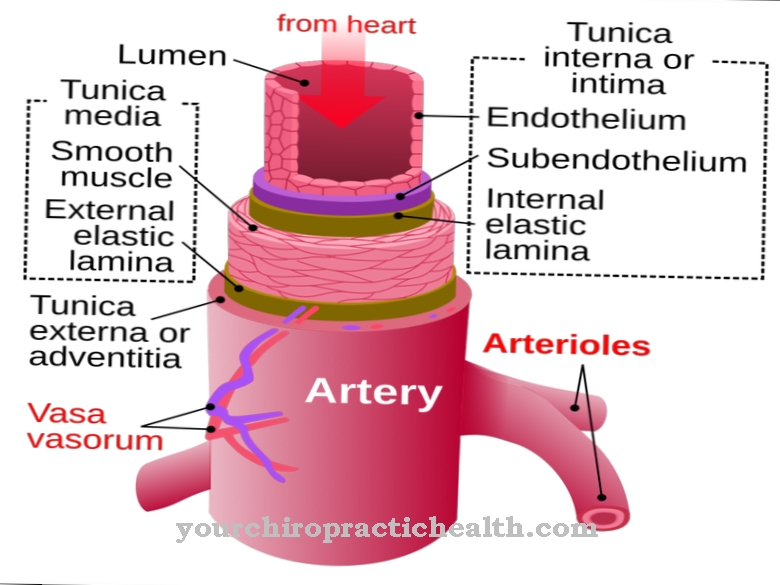
A great advantage of plexus anesthesia is that, in contrast to general anesthesia, it can be kept relatively minimally invasive. Due to the possibility of inserting a catheter, this anesthetic procedure can also be carried out over a longer period of time and used postoperatively to treat pain. Furthermore, the plexus anesthesia supports the healing process, since the anesthetic expands the blood vessels and thus the operating area is better supplied with blood and, if necessary, inflammation mediators and pain mediators can be transported away.
You can find your medication here
➔ Medicines for painRisks, side effects & dangers
Plexus anesthesia is generally a very safe form of anesthesia. The typical postoperative side effects, as with general anesthesia, do not occur with plexus anesthesia. There is no nausea or vomiting and since there is no need to intubate, there is no irritation of the throat or hoarseness.
The risks of plexus anesthesia are similar to those of local anesthesia. Thus, for example, allergic reactions to the anesthetic can occur. Long-term anesthesia may result in symptoms of poisoning in the form of dizziness, nervousness, seizures, cardiac arrhythmias or a drop in blood pressure.
When penetrating the plexus of nerves, it can happen that a vein or artery is damaged because they run in the middle of blood vessels. Postoperatively, side effects such as numbness, muscle tremors or tingling of the numb extremity can occur. Experience has shown, however, that these sensory disturbances subside after a few weeks. Bleeding (hematomas) may occur in the area of the puncture site and the surrounding soft tissue.
Furthermore, there can be general damage to the soft tissues or nerve irritation, despite adequate implementation and positioning. This damage or irritation can cause sensory disorders such as abnormal sensations, numbness, pain and even symptoms of paralysis. In response to the anesthetic, drops in blood pressure and pulse may occur. If the anesthetic is accidentally injected into blood vessels, it can lead to seizures, cardiovascular complaints, loss of consciousness and even breathing failure.
Plexus anesthesia is contraindicated if there is an infection or an allergy to anesthetics in the area of the injection.











.jpg)
.jpg)
.jpg)







.jpg)