In the Proctitis it is an extremely painful inflammation of the rectum and anus. Venereal diseases or systemic diseases such as ulcerative colitis or Crohn's disease are often the cause.
What is proctitis?

© Martha Kosthorst - stock.adobe.com
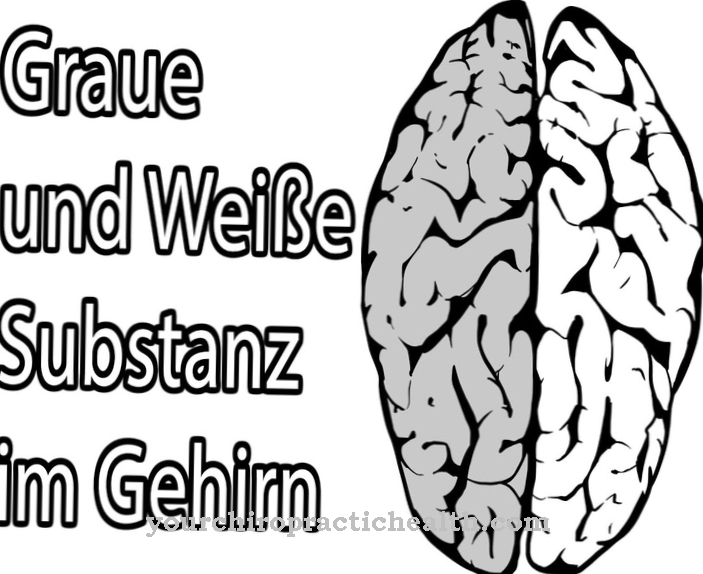
A Proctitis is an inflammation of the rectum.
While other inflammatory bowel diseases usually affect the entire intestine or large sections of the intestine, the inflammation in proctitis only affects the last six inches of the intestine. The causes of the disease are varied.
For example, bacterial infections, inflammatory bowel disease or allergic reactions are possible causes. Patients experience bloody discharge, pain, and an urge to defecate.
Proctitis can promote the development of anal polyps. These are enlargements of the anal papillae. They can grow up to two centimeters. When defecating, they slip out of the anus and then have to be pushed back with the finger. They often also cause a foreign body sensation in the intestines.
causes
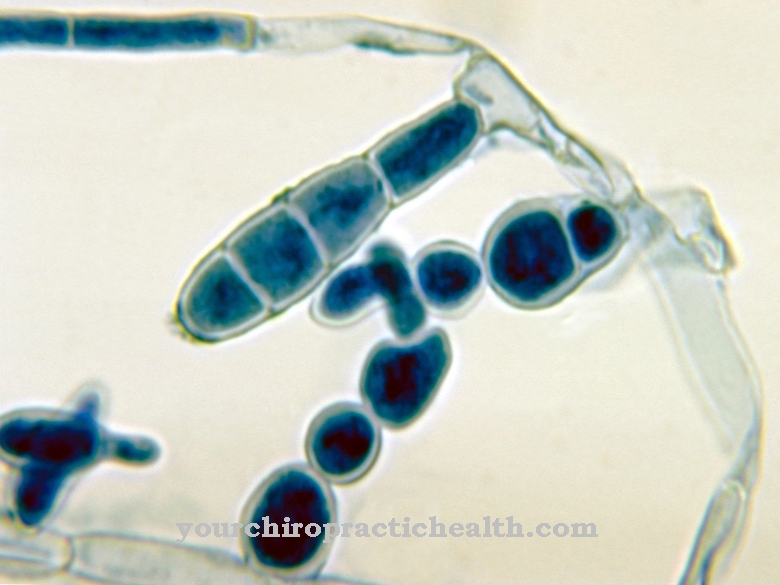
Infectious inflammation of the rectum occurs mainly in connection with sexually transmitted diseases. For example, with gonorrhea (gonorrhea), purulent proctitis occurs. Proctitis can also occur in the three stages of syphilis. Other sexually transmitted diseases that can be associated with the inflammation are ulcus molle, lymphogranuloma inguinale, AIDS, donovanosis, infections with Chlamydia trachomatis and herpes simplex virus infections.
The most common cause of infectious proctitis is unprotected, receptive anal sex. But also chronic inflammatory bowel diseases can affect the rectum. The best-known chronic inflammatory bowel diseases are ulcerative colitis and Crohn's disease. Ulcerative colitis spreads continuously from the anus to the mouth. Ulceration of the upper layers of the lining of the intestine occurs.
In Crohn's disease, the inflammation penetrates all layers of the intestine. However, here the spread is not continuous, but segmental. The disease preferentially affects the small intestine and the colon. Allergic or toxic reactions can also lead to proctitis. An allergic rash of the intestinal mucosa is caused, for example, by suppositories, condoms or lubricants.
A special form of a toxic reaction is the ergotism gangrenosus cutaneus. Here ulceration occurs after inserting ergotamine suppositories. These suppositories are used by migraine sufferers, for example. Other causes of proctitis are trauma or radiation therapy, for example in cancer.
Symptoms, ailments & signs
With proctitis, patients report watery, bloody, or purulent discharge from the anus. The stool can also contain bloody, purulent additions. There is severe itching in the anal region. Those affected tend to have irregular bowel movements, but constantly have the feeling that they have to go to the toilet.
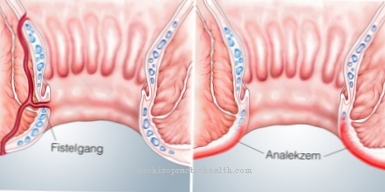
Often they cannot hold their stool, leading to fecal incontinence. Even air cannot be held in the intestine and escapes in an uncontrolled manner. This is also referred to as flatulence. The anus appears red and is protruded in a bulge. In the further course of the disease, anal fissures or fistulas can also occur in the anus. Anal fissures are tears in the skin or mucous membrane of the anus.
A fistula is a connection between an internal hollow organ and the surface of the body. In the case of proctitis, a tube-like connection forms from the rectum to the surface of the skin in the area of the anus. Both the anal fissure and the fistula are very painful. Depending on the type of infection, genital warts can also form. Which complaints actually occur depends on the cause. Proctitis caused by gonorrhea, for example, hardly causes any symptoms apart from a purulent discharge.
Diagnosis & course of disease
The symptoms provide the first signs of proctitis. If inflammation of the rectum is suspected, the doctor first inspects the anus. You may see bulges, redness, fistulas or fissures here. This is followed by the digital rectal examination (DRE). The rectum is palpated with the finger. If the inflammation is severe, this can be very painful.
A rectoscopy provides definite certainty. Before the examination, the patient must take a laxative so that the rectum is free of stool debris. The doctor then inserts an endoscope into the anus. He can use it to detect inflammation and bleeding and, if in doubt, treat it directly. Rectoscopy reveals inflammatory redness and infiltrated intestinal walls. You may also see erosions or ulcers.
For further clarification, the doctor can take smears or biopsies during the rectoscopy. Again, depending on the position of the endoscope, pain during the examination can occur.
Complications
Proctitis is a very unpleasant disease, but complications are rare. The specific cause plays a role here. Proctitis or rectal inflammation can spread to the entire intestine if it persists for a long time. Ulcer and chronic intestinal inflammation may develop, which significantly reduces the quality of life of the patient.
In particularly severe forms of proctitis, blood may be lost through bleeding in the rectum. This bleeding is particularly common with hemorrhoids. However, the intestinal inflammation does not affect the formation and development of hemorrhoids.
This happens especially with chronic inflammatory processes. In severe cases, blood loss sometimes leads to anemia (anemia). Typical symptoms for this are general paleness, weakness, shortness of breath, or dizziness. If the proctitis is left untreated, it can also lead to adhesions in the rectum area. Furthermore, the development of chronic fecal incontinence is also possible.
If the proctitis is caused by the so-called human papillovirus, genital warts sometimes develop. Although these usually heal completely, they can also break open and lead to bleeding. Some forms of proctitis are caused by sexually transmitted pathogens and are therefore highly contagious if left untreated.
When should you go to the doctor?
Irregularities in the area of the anus should be presented to a doctor. If symptoms persist for several days or if they increase in intensity, the person concerned needs medical help. Itching, pain, problems when using the toilet or a feeling of pressure in the bowel should be examined and treated. Those affected often report a foreign body sensation. This should be examined more closely by a doctor. In many cases, proctitis occurs as a side effect of a sexually transmitted disease. If this has not yet been diagnosed, a doctor should be contacted as soon as possible for clarification.
Swelling, difficulty moving or being seated are signs of an irregularity. A doctor's visit is necessary so that the cause of the symptoms can be found.If warts, growths or fistulas develop in the anal region, they should be examined by a doctor. Treatment is necessary so that there are no complications.
In the event of bleeding, impairment of the sphincter muscle activity or a loss of control over the activities of the sphincter muscle, it is advisable to see a doctor. Sufferers of proctitis can often no longer regulate the timing of the excretions independently. Therefore, they should seek medical help. If there are disturbances within the sexual act or a decrease in libido, these are also indications of a health impairment.
Therapy & Treatment
Therapy depends on the cause. Bacterial infections are treated with antibiotics. The treatment of chronic inflammatory bowel diseases is a little more difficult. Immunosuppressants, TNF-alpha blockers and other drugs are used here.
In severe cases, pieces of the intestine must be surgically removed. If the proctitis is based on an allergic reaction, the trigger should be avoided urgently in the future. Anti-inflammatory enemas or suppositories are used for symptomatic treatment.
prevention
Infectious proctitis can be prevented with condoms. In particular, people who often have anal intercourse with changing people should always use condoms. Inserting objects into the anus can also lead to inflammation through small tears in the intestinal mucosa. Sex toys should therefore be used extremely carefully in this area. If there are known allergies to certain medications or substances (e.g. latex), these should of course be avoided as much as possible.
Aftercare
Whether follow-up treatment is necessary also depends on the severity and cause of the disease. For example, if it is an infection-related proctitis, some check-ups may be necessary. These are carried out regularly, depending on the severity of the proctitis.
If the disease has only taken a mild course, no further checks by the doctor are necessary. If the course is moderate or severe, however, the doctor should check after the treatment whether it was successful. The first of these examinations usually takes place one to two weeks after the start of therapy. For this purpose, further smears are taken from the intestinal wall and checked.
If no infection can then be detected in these, the therapy was successful. Until success is confirmed, no further sexual intercourse should be undertaken that could irritate the anus or rectum. Otherwise, after the successful treatment of infectious proctitis, no further follow-up treatment is necessary.
However, if proctitis is caused by inflammatory bowel disease such as ulcerative colitis, patients can be affected for a long time. This means that they have to be treated with medication over the long term. Meanwhile, those affected should also visit their doctor regularly and have check-ups carried out.
You can do that yourself
Proctitis is an acute or chronic inflammation of the rectum. The lining of the rectum is considered to be very sensitive, which should be taken into account in any type of self-treatment or self-help. In many cases the proctitis is bacterial, so antibiotics are usually required. In many cases, those affected make the mistake of not performing antibiotic therapy long enough or in too low a dose. Since an irregular intake of antibiotics can cause pathogen resistance, the result is often chronic disease. In addition to antibiotics, other medications prescribed by a doctor, such as immunosuppressants or antiallergic drugs, should always be taken strictly according to medical instructions for chronic proctitis.
In rare cases, proctitis is based on an allergic event, in which case the allergic trigger should be avoided as much as possible in the future. Suppositories or so-called enemas can also be used for symptomatic treatment. Often, infectious proctitis occurs in people who regularly practice anal intercourse. For this reason, condoms should always be used as a preventive measure, especially if the sex partner changes frequently. Inserting sex toys into the anal canal can also lead to microcracks on the sensitive mucous membrane and thus to proctitis. If you are allergic to latex, you should only use sex toys that are guaranteed to be latex-free.



.jpg)





.jpg)





.jpg)