A Inflammation of the prostate (prostatitis) can come in different forms. Most men suffer from acute inflammation of the prostate gland. If this disease occurs frequently or if it is not adequately treated, it can lead to chronic prostate inflammation (prostatitis). Typical signs are burning and drawing pains when urinating, fever and chills.
What is Prostate Inflammation?
.jpg)
© designua - stock.adobe.com
The man's prostate is responsible for producing some of the sperm. Like any other organ, however, it can become inflamed:
This is called Prostate inflammation, also known as Prostatitis designated. In a broader sense, it also describes all other inflammations of the pelvic floor that cannot be assigned to any other cause.
Typical symptoms include difficulty and pain when passing urine, increased urination, and severe pain after ejaculation.
causes
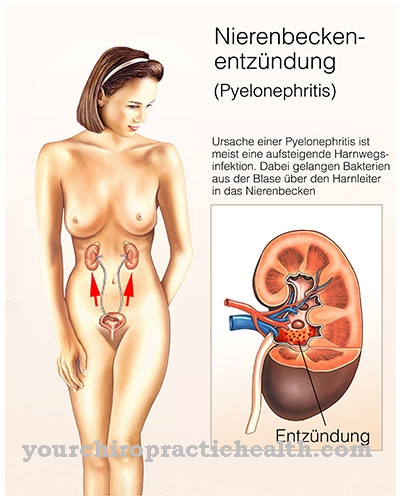
The acute Inflammation of the prostate (prostatitis) is the body's response to bacterial infections. In most cases these are intestinal bacteria of the type E. coli, which can be detected in large quantities in the urine of affected men. Other, but rarer, triggers are chlamydia or various mycoplasmas. If the bacterial prostate inflammation has become chronic, other bacteria usually also play a role.
For example, Mycobacterium tuberculosis was identified as a possible trigger, which must have been preceded by genital tuberculosis. Viruses and fungi are less commonly associated with chronic prostatitis.Usually the cause is that the trigger of the previous acute illness remained in the urethra and after the first episode of infection was healed, it returned to the prostate, which was still weakened.
Abacterial prostate inflammation (prostatitis) is by far the most common manifestation. It hardly differs from bacterial inflammation, but it has other causes. Neural disorders through to autoimmune reactions are possible. Although it is discussed that bacteria that are difficult to detect could act as pathogens, there is no evidence for this.
Symptoms, ailments & signs
Acute prostate inflammation usually begins with a general feeling of illness. The patient feels tired and exhausted, and develops a fever with chills. Urination causes burning pain, much like a cystitis. The urine stream can be restricted by the swollen prostate.
Because little urine can be excreted when using the toilet, the patient often has the urge to urinate. There is also pain in the perineal area, which can radiate into the penis, testicles, bladder and groin. Pain can also occur during bowel movements and sexual intercourse, especially during or after ejaculation.
A purulent encapsulation (abscess) in the prostate is possible as a complication of acute inflammation. It must be surgically opened and removed. The chronic inflammation of the prostate causes less severe discomfort. There is no fever and no chills. The strongest symptom is a feeling of pressure in the perineum or abdomen.
The ejaculate may be brown in color due to traces of blood. Blood in the urine is also possible. Even in the chronic form, men often feel more painful during or during ejaculation. In addition, it can lead to libido or potency disorders. If the inflammation is not treated, it can spread to surrounding organs, such as the testicles or the epididymis.
Course of disease
In an acute one Inflammation of the prostate (prostatitis) A prostate abscess or urinary retention can occur as complications in the course of the disease. If a chronic form of prostate inflammation (prostatitis) has already occurred, new infections can occur again and again, so that treatment can be very lengthy and complicated.
Complications
Recognized and treated in good time, acute prostate inflammation heals in most cases within a short time without consequences. Occasionally, the triggering bacteria get into the testes and cause epididymitis there. A further complication can be a prostate abscess, in which pathogens encapsulate themselves in the prostate and cause massive purulent inflammation.
This can be accompanied by fever, chills, and severe pain in the affected area. A prostate abscess is usually surgically opened immediately, as the pus focus can otherwise break into the urinary bladder, urethra or rectum. Furthermore, urination disorders are possible as a consequence of prostatitis, which can extend to complete urinary retention - in this case, urination must be performed with the help of a catheter.
A rare but life-threatening complication is blood poisoning (urosepsis), in which bacteria enter the bloodstream and spread throughout the body. If treatment is not given promptly, vital organs will fail. Acute prostatitis that is inadequately treated with antibiotics often turns into chronic prostate inflammation: the infection flares up again and again and must be treated with medication. If the antibiotic is discontinued too early, there is a risk of resistance building up, in which the triggering bacteria no longer respond to the active ingredient.
When should you go to the doctor?
Symptoms such as a burning sensation when urinating, an increased need to urinate and an uncomfortable feeling in the lower abdomen indicate an inflammation of the prostate. A doctor's consultation is necessary if the symptoms do not subside within two to three days. If there are general symptoms such as fever or malaise, it is best to consult your family doctor immediately. Sometimes the symptoms appear in connection with a bacterial infection or tuberculosis of the genital organs. Then the responsible specialist should be called in.
The same applies if the health problems arise in the context of a chlamydia infection. Apart from the family doctor, you should go to a urologist with an inflammation of the prostate. In the case of organic causes, the responsible specialist must be consulted so that treatment can be started quickly. If no physical cause is found, the suffering may be psychological. The patient should see a psychologist or psychotherapist if mental health is poor or if there is any suspicion that a psychological trigger is present.
Treatment & Therapy
The acute Inflammation of the prostate (prostatitis) is first treated with antibiotics. Depending on the pathogen, different preparations come into question. The chronic form is also treated with antibiotics, but other drugs are used. In order to combat the chronic bacterial inflammation of the prostate, gentler means are required, since the administration of antibiotics can extend over 4-6 weeks. In addition, alpha blockers or prostate massages are often prescribed to help limit the painful symptoms.
Abacterial prostatisis is more difficult to treat. It must first be determined whether it is an inflammation or not. In some cases, the pain can also be caused by unhealthy tension in the muscles of the pelvic floor and affect the prostate only among other things, sometimes not at all. The administration of antibiotics has been shown to help prevent bacterial inflammation of the weakened area. However, quercetin, alpha-1 blockers or mepartricin play the main role in drug treatment.
prevention
One Inflammation of the prostate (prostatitis) It is hardly possible to prevent effectively, as it is based on internal processes in the body over which humans have little influence. In principle, thorough personal hygiene and compliance with hygienic principles help to let the pathogens of inflammation penetrate the body through the urethra.
A chronic prostate inflammation can be prevented by having the acute form treated by a doctor immediately. Antibiotics must be taken down to the last tablet in the pack or as directed by the doctor, as otherwise the bacterial population cannot be completely killed. If the symptoms recur or if there is only slight improvement, the doctor must be consulted again immediately.
Aftercare
Follow-up care for prostate inflammation takes place a few days after recovery. If the patient is no longer in pain and has otherwise not noticed any unusual symptoms, the responsible urologist is consulted. Follow-up care includes a physical exam and a patient interview. During the physical exam, the doctor will check the bladder region.
Typical symptoms such as inflammation of the epididymis or fever are clarified. If the symptoms persist, a blood test may be necessary. Other typical symptoms that are difficult for the doctor to see during the physical examination are clarified in the patient consultation. These include the typical painful urination and general potency problems.
If no abnormalities are found, the treatment can be concluded. A prescribed antibiotic must be tapered off. The doctor may prescribe a lighter medication or refer the patient to an alternative doctor.
Follow-up care for prostate inflammation is carried out by the urologist who has already taken on the treatment. It is a one-time examination aimed at clarifying the symptoms. Once the patient has recovered completely, no further visits to the doctor are necessary. Before discharging, the doctor can advise the patient about preventative measures to prevent re-inflammation of the prostate.
You can do that yourself
Bacterial prostatitis is very often caused by pathogens that travel from the urinary tract to the prostate and kidneys. For this reason, countermeasures should be taken immediately at the first signs of urinary tract disease.
Patients help themselves best by flushing their urinary tract thoroughly in order to flush out the germs and keep the bacterial concentration as low as possible. You should drink plenty of water or unsweetened herbal or fruit tea for this. In pharmacies and drugstores there is also special bladder tea that not only flushes the urinary tract, but also has a pain-relieving effect. In naturopathy, pumpkin seeds and drops and tablets based on them are also used.
If the prostatitis is chronic, the patient can improve his chances of recovery by protecting himself from hypothermia. Wear appropriate clothing for the weather, warm underwear and avoiding cold seats. Warm hip baths can also relieve tension and relieve pain. In addition, the patient can learn and use relaxation techniques such as yoga or tai chi, which also has a beneficial effect on chronic tension pain in the pelvic area. If the patient also suffers from erectile dysfunction, he should definitely point this out to his treating doctor and not remain silent out of shame, as this makes diagnosis and therapy more difficult.

.jpg)
.jpg)








.jpg)

.jpg)
.jpg)











.jpg)