At a Pyaemia it is a particularly severe form of blood poisoning (sepsis), in which the germs transported by the blood flow also attack other organs secondarily. The prognosis is generally even worse than that of ordinary sepsis.
What is pyaemia?

© greenvector - stock.adobe.com
The Pyaemia is also known as general metastatic infection referred to because masses of pathogens infect other organs via the bloodstream. The pathogens spread across the bloodstream in a similar way to the cancer cells in a cancerous tumor. In this sense, pyaemia can be viewed as a particularly severe form of sepsis.
Even the usual sepsis is a serious clinical picture. It is characterized by complex systemic inflammatory reactions due to a massive infection with bacteria, bacterial toxins and fungi. In the case of pyaemia, however, pathogens also get into the lungs, heart, spleen, liver, kidneys, joints or brain via the blood as part of an emboli-like spread.
There, too, foci of infection develop, which in turn can spread and exacerbate the entire disease process. Abscesses form all over the body. A typical example of pyaemia is puerperal fever. In puerperal fever, various pathogens penetrate the organism through a large wound area in the placenta and cause inflammation in the peritoneum, uterus, intestines and other organs. In this context, it should be noted that the discoverer of puerperal fever, the Hungarian doctor Ignaz Philipp Semmelweis, himself died of pyemia in 1865.
causes
Pyemia is caused by the massive entry of pathogens such as Streptococcus pyogenes, Staphylococcus pyogenes, Staphylococcus aureus or Neisseria into the bloodstream. These spread throughout the organism and cause the symptoms of sepsis, which is accompanied by an additional infection of other organs. Thus, in the case of pyaemia, the organism is impaired both by the systemic inflammatory reactions and by the additional infestation of other organs with germs.
In the case of childbed fever, for example, these pathogens enter through the cervix opened during the birth process. There is a direct connection from the vagina to the uterus via the cervix. Even with good hygienic conditions, it is easy for the pathogens to infect the uterus. However, the weekly flow usually ensures that the germs are transported back.
However, this is not the case if the weekly flow is too weak and the after-pains are too weak. Other forms of pyaemia are also transmitted through wounds. Both the development of sepsis and pyaemia depend on three factors. These factors include the virulence of the germs, the state of the immune system and the type of reaction of the organism. It also plays a role where and how the pathogens enter the organism.
They immediately get into the blood through wounds. Organs such as the brain, lungs or abdominal cavity are poorly protected even in the case of harmless infections, so that the germs can spread quickly there. People with a weakened immune system naturally have a higher risk of developing sepsis or even pyaemia. If a large number of pathogens enter the bloodstream, however, a strong immune system often no longer helps to avert pyaemia.
Symptoms, ailments & signs
Like sepsis, pyemia is characterized by high intermittent fever, increased respiratory rate, severe impaired consciousness, diarrhea, nausea, vomiting, chills, high heart rate, very low blood pressure and possibly septic shock. Abscesses form all over the body. If left untreated, pyaemia always leads to death.
Diagnosis & course of disease
In diagnostics, the examination of the causative pathogens and the origin of the infection is particularly important. Blood cultures are grown to determine the pathogen. A blood count must also be taken. As part of a blood gas analysis, statements can be made about the gas distribution of carbon dioxide and oxygen as well as the acid-base balance.
Various parameters must be checked during pyaemia. These include regular blood culture examinations, blood pressure controls, blood gas determinations, lung function tests and much more.
Complications
In the worst case, pyemia can lead to death. However, this usually only occurs if the disease is not treated. The internal organs are attacked by the pathogens and can thus be irreversibly damaged. The patients suffer from a very high fever due to the pyaemia. The fever does not go away with the help of medication.
The respiratory rate of those affected is also not infrequently disturbed in pyaemia and there are disorders of consciousness and possibly also a loss of consciousness. In most cases, those affected also experience nausea or vomiting. In addition to the fever, shaking forests also occur and those affected suffer from high blood pressure. If left untreated, the pyaemia usually leads to death.
There are usually no special complications in the treatment of pyaemia. The disease can be treated relatively well with the help of antibiotics. The earlier the disease is diagnosed and treated, the better the chances of a complete cure for the patient. In severe cases, organ transplants may be necessary.
Treatment & Therapy
Since pyaemia is an emergency situation, treatment must be started before the pathogen has been fully identified. The earlier therapy begins, the greater the likelihood of survival. A wide range of antibiotics must first be administered in order to reach the full spectrum of pathogens.
After the resistance test, you can switch to the specifically adapted antibiotic. The focus of infection must also be surgically sanitized. This also applies to the removal of abscesses in the other organs. It is also necessary to adjust the central venous pressure and the mean arterial pressure by means of infusions.
Other treatment methods also include the administration of erythrocytes and lung ventilation. Often other organ-supporting measures have to be carried out. Despite the most intensive therapy, over 30 percent of the sick die.
prevention
To prevent pyaemia, the risk of infection should be reduced. It is important to strengthen the immune system in general to protect yourself against infectious diseases. A healthy lifestyle with a balanced diet, plenty of exercise and little stress are recommended.
The consumption of alcohol and smoking should also be restricted. Furthermore, compliance with hygienic standards such as hand washing and disinfection is very important. This is particularly true when it comes to contact with seriously ill people. To avoid childbed fever, births should always take place under medical supervision.
Aftercare
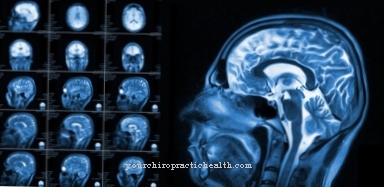
If pyaemia has been successfully treated, good follow-up care is important to avoid recurrence of pyaemia or sepsis (blood poisoning) and secondary diseases such as organ damage. The organs affected by the pyaemia should be examined regularly. Depending on the organ, this is done with imaging methods such as ultrasound, MRI, CT and X-rays.
However, only external organ damage can be detected and the healing of the damage caused by the pyemia can be monitored. The organ function should, however, also be monitored, since restrictions are possible in the long term as a result of pyaemia. This is done by regularly checking the organ values in the blood. If the brain has been affected by the pyemia, long-term effects can often not be detected by blood tests.
The emergence of neurological symptoms such as new headaches that occur for no apparent reason, muscle tremors or paralysis can be a long-term consequence of pyaemia and should be clarified with the attending physician immediately after the first occurrence. Organ damage that has already occurred must also be treated separately after the pyaemia has been treated.
If the underlying disease is an inflammatory skin disease, it must be treated dermatologically over the long term. If such an underlying disease is present, a high standard of hygiene should also be observed to prevent bacteria from spreading on the skin.

.jpg)
.jpg)







.jpg)

.jpg)
.jpg)











.jpg)