As Reabsorption is the re-absorption of water and nutrients from the kidney back into the bloodstream.
What is reabsorption?
Reabsorption is an important kidney activity. It takes place in the nephrons during urine production: The first part of reabsorption takes place after the blood has been pressure-filtered. With pressure filtration, the blood flows through the highly permeable capillaries of the glomeruli and is freed from waste materials. In addition to waste materials, numerous important molecules such as amino acids, glucose and water are also filtered out. The subsequent reabsorption, also known as selective reabsorption is called, the useful components are reabsorbed from the proximal tubule, i.e. the adjoining part of the nephron.
The second part of the reabsorption takes place after the tubular secretion and, together with the excretion of the concentrated urine, forms the end of the filtration process. This part of the reabsorption is also known as water reabsorption, since large parts of the water present diffuse from the collecting pipes back into the nephron and then participate in the circulatory system again.
The kidneys make use of the physical laws of osmosis for the reabsorption of water and first of all absorb the sodium present. Since water is always attracted to salt, the reabsorption of the salt causes the water to migrate back into the nephron and return to the bloodstream via the renal vein.
This completes the blood filtering process and the resulting urine is excreted from the kidney and passed on to the urinary bladder (excretion).
Function & task
The process of reabsorption is an important part of kidney activity, as it is vital for the human organism. The kidney filters around 1800 liters of blood daily and uses it to produce 180 liters of primary urine, which it in turn minimizes to two liters of terminal urine through reabsorption.
Anyone who has left 180 liters of primary urine within 24 hours knows how to marvel at the reabsorption capacity of functioning kidneys. Furthermore, in addition to the enormous amount of urine to be drained in the case of non-resorbing nephrons, there would also be an enormous amount of water that would have to be absorbed. It is estimated that around 7 liters of water would have to be added every hour to compensate for the enormous water loss.
The reabsorption processes also have a great influence on blood pressure. A high level of reabsorption can lead to pathologically increased blood pressure. At the same time, a constant blood pressure is necessary to ensure efficient pressure filtration in the glomeruli of the kidneys. A lowered blood pressure can therefore have a pathogenic effect on the filtration processes of the kidneys.
Due to the enormous importance of constant pressure in the bloodstream, there are several regulatory mechanisms in the body that control the resorption processes of the kidneys. The renin-angiotensin system influences the reabsorption processes of the kidneys via hormonal information carriers. Measurement points for the hormonal information network are contained in the liver, kidneys and capillaries of the lungs.
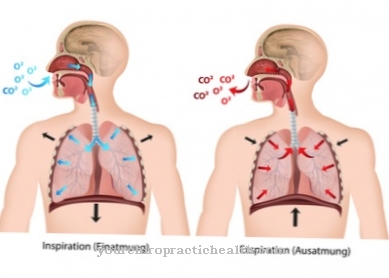
An increase in blood volume and thus blood pressure is initiated via the liver. Angiotensinogen is made here and passed on to the kidneys. If the blood pressure in the nephrons of the kidney is also too low, renin is produced here, which converts the angiotensin into angiotensin I. The angiotensin I is then transported to the capillaries of the lungs via the bloodstream. If the blood pressure also appears too low here, the lungs secrete the angiotensin converting enzyme (ACE), which converts angiotensin I into angiotensin II.
The angiotensin II is in turn sent to the kidneys, causing the adrenal glands to release the hormone aldosterone. Aldosterone promotes sodium reabsorption and thus also the reabsorption of the water, which inevitably leads to an increase in blood pressure. The organs are thus connected to one another via a hormonal information network.
Illnesses & ailments
Hormonal disorders in the absorption process can trigger serious diseases. One of these diseases is called diabetes insipidus. Here will as a result of the lack of reabsorption, too much unconcentrated urine is excreted and the body begins to dry out. Hypernatremia or hypertonic dehydration will quickly develop if large amounts of water are not constantly supplied. Salts and other electrolytes collect in a highly concentrated form in the bloodstream and further promote dehydration.
Diabetes insipidus is divided into two forms: Diabetes insipidus centralis describes a form in which the antiduretic hormone ADH is inadequately produced in the hypothalamus or inadequately transported. The ADH promotes the reabsorption of water in the collecting pipes and counteracts the excretion. In contrast, an insufficient amount of ADH is a sign for the kidneys that reabsorption is not necessary. Diabetes insipidus centralis can be hereditary or be a consequence of a traumatic brain injury. No causal conditions can be determined in a third of all sick people. For the unexplained cases of illness, as yet unresearched autoimmune diseases are given as causes.
In diabetes insipidus renalis, the defect is not in the hormonal production or transmission of the antidiuretic hormone, but in the kidney itself. In spite of the correct hormonal control, the kidney is not able to guarantee a reabsorption process and consequently cannot excrete concentrated urine. The causes that can be responsible for kidney failure are manifold. Drugs like lithium or defective kidney tubules are just two of the many reasons for severe kidney failure.










.jpg)

.jpg)
.jpg)











.jpg)