Rifabutin is counted among the tuberculostatics. These are special antibiotics for treating tuberculosis.
What is rifabutin?

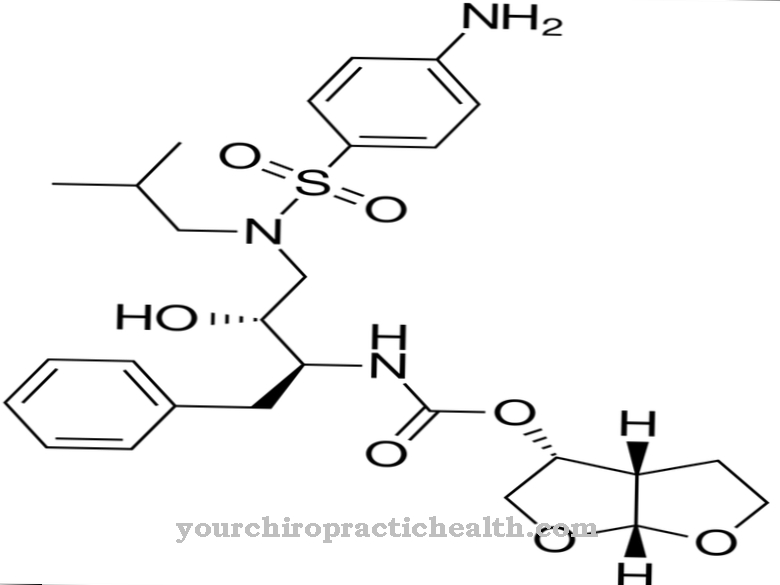
Rifabutin is an antibiotic that belongs to the group of antibiotic bactericides. It is sold under the trade name Mycobutin® and is a semi-synthetic rifamycin derivative. This is suitable for the treatment of mycobacteria as well as gram-positive and gram-negative infections.
Rifabutin belongs to the group of tuberculostatics. This means that the drug is specifically used to treat tuberculosis. As a rule, tuberculosis treatment is carried out in combination with other tuberculosis drugs such as rifampicin, isoniazid, ethambutol or pyrazinamide in order to counteract the development of resistance.
Rifabutin was approved in Europe in the mid-1990s. The active ingredient has been on the list of essential drugs of the WHO (World Health Organization) since 2011.
Pharmacological effect
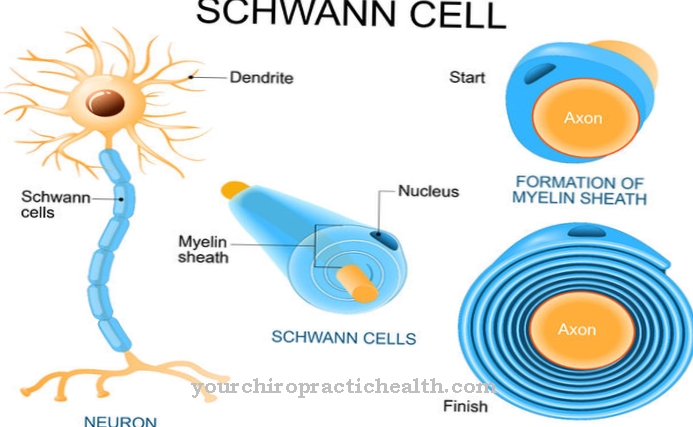
The way rifabutin works is similar to that of rifampicin. Rifabutin also inhibits the DNA-dependent RNA polymerase of sensitive bacteria, which leads to a blockage of the protein synthesis of the germs. There are also indications that the DNA synthesis of the bacteria is also affected.
In some cases, rifabutin can also exert its positive effect against Mycobacterium tuberculosis strains that are resistant to rifampicin. In contrast to rifampicin, the activity of rifabutin is significantly higher, which is due to the inhibition of the RNA polymerase. While around 94 percent of all mycobacteria are resistant to rifampicin, it is only around 20 percent for rifabutin, which is another advantage of the tuberculostatics. In addition, rifabutin has biological activity against the Heliobacter bacterial genus.
If rifabutin is taken by mouth, its effects are enhanced by the simultaneous ingestion of protein-containing foods. The metabolism of the antibiotic takes place partly through the liver. 85 percent of the rifabutin is bound to protein. Rifabutin reaches its highest level in the organism's blood plasma level after a period of about six to eight hours. Most of the active substance escapes from the body via the kidneys. The half-life of tuberculostatics varies between 28 and 62 hours.
Medical application & use
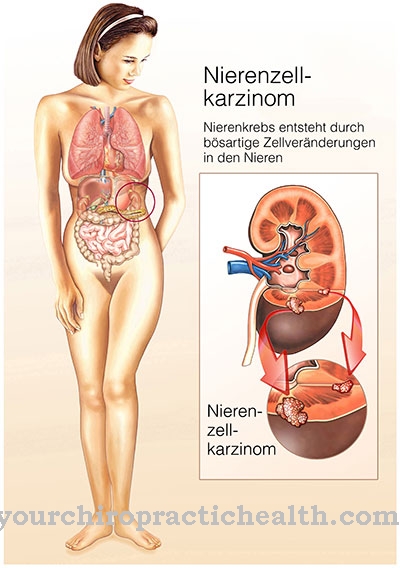
Rifabutin is used to prevent infection with Mycobacterium avium-intracellulare (MAI) in AIDS patients. Treatment for MAI infections is also possible. This is done in combination with other antibiotics such as ethambutol, azithromycin and clarithromycin. Medicine also uses rifabutin to treat multidrug-resistant tuberculosis.
Rifabutin also acts against bacterial pathogens such as Mycobacterium paratuberculosis, Mycobacterium leprae and Chlamydia pneumoniae. Therapy of the chronic inflammatory bowel disease Crohn's disease is also possible.
The usual dose for taking rifabutin is 450 to 600 milligrams of rifabutin per day. However, if clarithromycin is administered concurrently, the daily dose is reduced to 300 milligrams. The duration of treatment is usually six months. For the prophylaxis of MAC infections (Mycobacterium avium complex) in AIDS patients, the usual daily dose is 300 milligrams. In order to prevent the development of resistance, it is advisable to exclude infections with mycobacteria in advance.
If the patient has previously received other tuberculostatics, an increase in the dose to 300 to 450 milligrams is recommended. Increasing the dose is particularly useful in patients who are immunosuppressed. Rifabutin can be taken at any time of the day and independently of meals. The capsule is taken once a day.
You can find your medication here
➔ Medicines against coughs and coldsRisks & side effects
When using rifabutin, undesirable side effects are possible. They are similar to the side effects of taking rifampicin. This often leads to an increase in liver enzymes, nausea and vomiting. Other possible side effects may include skin rash, upper abdominal pain, diarrhea, chest pain, changes in taste, migraine-like headache, sore throat, flu-like symptoms, bruising, anxiety or jaundice. Sometimes stool, urine, sweat, tear fluid and saliva turn orange-brown during the rifabutin treatment.
Rifabutin should not be taken if the patient is hypersensitive to the active ingredient. There is therefore a risk of bronchospasm, eosinophilia (a special form of leukocytosis) or shock. Combination treatment with clarithromycin also increases the risk of iris inflammation (uveitis).
A disadvantage of rifabutin is the high likelihood of interactions with other drugs, such as those used to treat AIDS. So it is possible that the effect of the preparations is weakened. The agents affected include anticoagulants, pain relievers such as opioids, hormonal contraceptives, glucocorticoids and the active ingredients phenytoin, digitoxin, cotrimoxazole and dapsone.
The mode of action of rifabutin can in turn be impaired by the simultaneous administration of drugs such as cimetidine, erythromycin, clarithromycin, ketoconazole and fluconazole.





.jpg)