The Renal cell carcinoma is a malignant tumor that originates in the tubular cells of the kidneys. The majority of all kidney tumors are renal cell carcinomas.
What is renal cell carcinoma?

© Henrie - stock.adobe.com
About three percent of all malignant tumors in adulthood are kidney carcinomas. Every year nine out of 100,000 residents get sick with one Renal cell carcinoma. Most people get sick between the ages of 40 and 70. Renal cell carcinoma, also known as Grawitz tumor has its origin in the tubular cells of the kidney.
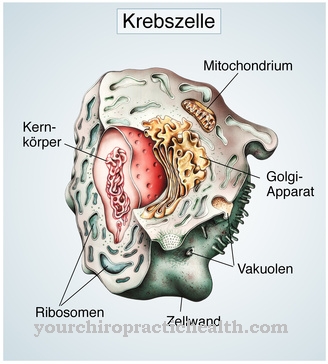
Depending on the initial tissue, cytogenetic findings and histological picture, different renal cell carcinomas can be differentiated. Classic renal cell carcinoma occurs most frequently. It is also called Clear cell carcinoma designated. Other forms of renal cell carcinoma are the chromophilic or papillary carcinoma and the chromophobic carcinoma. Bellini duct carcinoma develops rather rarely. It is also known as collector tube carcinoma.
causes
The exact etiology of renal cell carcinoma is still unclear. It is known that men fall ill more often than women. Patients who suffer from Hippel-Lindau syndrome often fall ill. Hippel-Lindau syndrome is an autosomal dominant inherited disorder that is associated with vascular malformations in the face and the central nervous system.
Risk factors for renal cell carcinoma are old age, chronic renal insufficiency, smoking, exposure to lead, exposure to cadmium, long-term therapy with painkillers, congenital tuberous sclerosis and contact with trichloretes.
Symptoms, ailments & signs
Renal cell carcinoma usually only causes symptoms when the tumor is already quite large. There are usually no early symptoms. The tumor cells initially grow centrally in the parenchyma and thus have no connection to the tubular system of the kidney.
An early stage renal cell carcinoma is therefore often only an incidental finding during an ultrasound examination of the abdominal organs. Almost 70 percent of all kidney tumors are found by chance during imaging examinations such as sonography, computed tomography or magnetic resonance imaging. Blood in the urine is a characteristic and threatening late symptom of renal cell carcinoma. This hematuria is sudden and painless.
Other symptoms of renal cell carcinoma are rather unspecific. The tumor can cause pain in the flank. Particularly pronounced tumors can be felt in the flank area. So-called B symptoms can occur in the context of cancer. These include weight loss, an increased susceptibility to infections, night sweats and fever. Those affected are no longer as productive as they used to be.
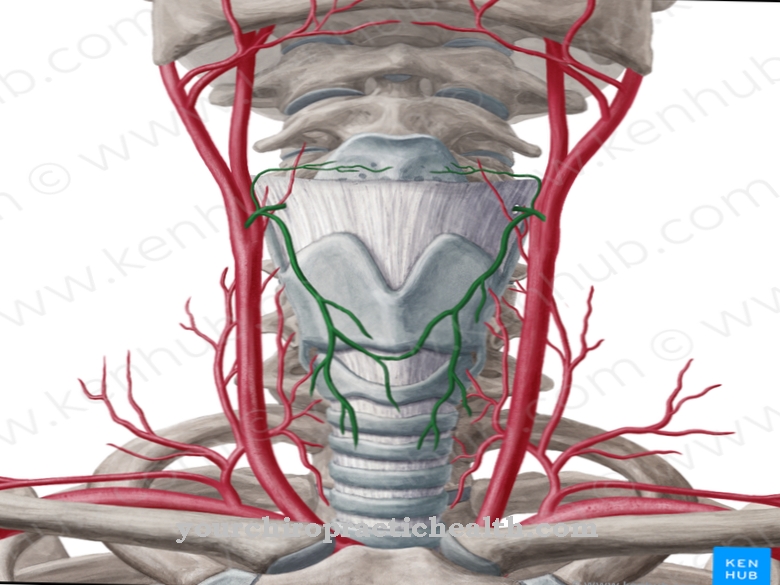
It may lead to anemia with tiredness, hair loss, difficulty breathing when exerted and very pale. If the tumor grows into the left renal vein or compresses the left renal vein, a varicose vein can develop on the testicle in men. This is also known as a varicocele.
Paraneoplastic syndrome rarely develops in renal cell carcinoma. Paraneoplastic syndrome is the term used to describe the symptoms accompanying cancer that are not caused by the tumor. In renal cell carcinoma, the paraneoplastic syndrome can be caused by tumor cells that produce hormones such as renin, erythropoietin, ACTH or parathyroid hormone.
Possible symptoms of such a paraneoplastic syndrome are high blood pressure, hyperthermia, and cachexia. There is a possibility that Cushing's syndrome will develop due to the increased ACTH level. Those affected have a full moon face, gain weight, have a so-called bull's neck and suffer from weak muscles and heart.
Diagnosis & course of disease
During the clinical examination with palpation, auscultation and percussion, only large and very advanced tumors of the kidneys are found. Hematuria is indicated by the urine turning pink. With the help of a urine stick, erythrocytes can be detected in the urine. The laboratory may show anemia, which is caused by the large amount of blood lost through the kidneys.
To confirm the diagnosis, however, an ultrasound examination must be carried out. With the help of sonography, suspicious masses in the kidney are diagnosed. The conspicuous areas are then punctured. The tissue material obtained is examined histologically by a pathologist. Most renal cell carcinomas have a lipid-rich and glycogen-rich cytoplasm.
Computed tomography of the abdomen is performed to assess the growth of the tumor, known as staging. The CT can also be used to determine the operability of the cancerous tumor.Distant metastases can be detected with chest x-rays, skeletal scintigraphy, and brain MRI.
However, only metastases that are larger than one centimeter in diameter are recorded in the X-ray image. The 5-year survival rate for patients with renal cell carcinoma is around 50 percent.
Complications
Renal cell carcinoma can lead to severe complications, which is typical for tumors. In a large number of patients, this leads to progressive metastasis of other organs. This is because malignant kidney tumors tend to spread through the body via the lymph and blood vessels and form daughter tumors. In particular, the lungs, liver, brain and skin can be attacked by other tumors.
Metastasis of the bones is also within the typical spectrum. As a result, life-threatening complications can arise from renal cell carcinoma, such as clots (embolism), blocked blood vessels or pneumonia. The likelihood of metastasis in other organs increases significantly if renal cell carcinoma is not treated or treated very late. This is one of the reasons why early detection plays an important role.
In the course of medically indicated treatment, complications can also arise that can be traced back to the substances ingested. Occasionally, the antiangiogenic antibody bevacizumab leads to thromboembolic events and perforations in the gastrointestinal tract.
When should you go to the doctor?
Renal cell carcinoma symptoms are often silent in the early stages of the disease. If the disease progresses, individual symptoms can become noticeable. If you experience unreasonable weight loss or flank pain that becomes worse, you should see a doctor.
Fever that lasts for a long time should always be clarified by a doctor. A significant and long-lasting decrease in performance can be the symptom of a serious illness. In such a case a doctor should be contacted. Blood in the urine is also a reason to see a doctor. Seeing a doctor early can have a positive effect on the prognosis. If you are unsure, a doctor's appointment should be made as soon as possible.
Therapy & Treatment
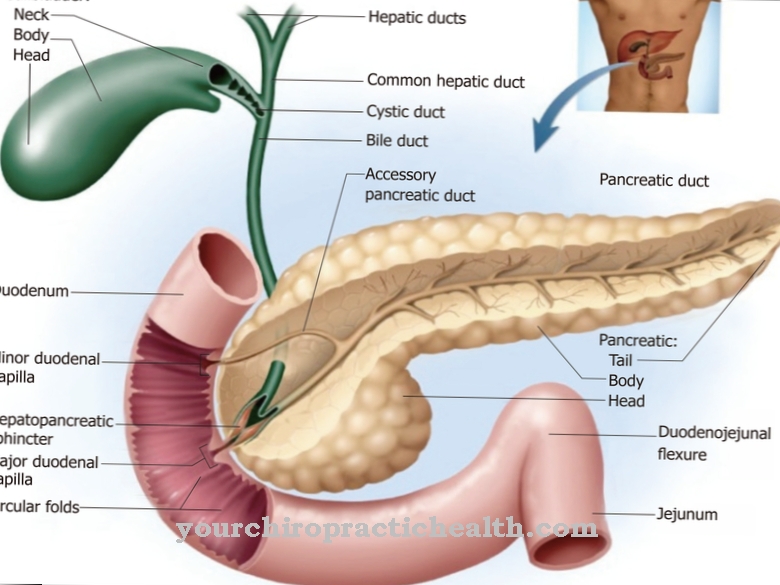
The gold standard in the treatment of non-metastatic renal cell carcinoma is surgical removal. Tumors no larger than seven centimeters are usually removed while preserving the kidneys. For larger tumors, the entire kidney along with the adrenal gland, ureter, kidney capsule and surrounding fatty tissue must be surgically removed.
If the tumor has grown into the renal vein or even the inferior vena cava, these tumor cones must also be removed. The use of a heart-lung machine may be necessary. New surgical procedures such as laparoscopic radical nephrectomy or minimally invasive procedures such as radiofrequency interstitial tumor ablation (RITA) are currently being researched and tested.
Drug therapies are used for metastatic and locally inoperable renal cell carcinomas. Drug therapies for renal cell carcinoma are usually palliative; a cure is usually no longer possible. Classic cytostatics such as antimetabolites, alkylating agents, anthracyclines and mitosis inhibitors are ineffective in renal cell carcinoma.
Renal cell carcinoma is therefore considered to be chemotherapy-resistant. Cancer immunotherapies are used instead of chemotherapy. Oral tyrosine kinase inhibitors, bevacizumab and mTOR inhibitors are also used.
Outlook & forecast
The prognosis for renal cell carcinoma depends largely on the time of detection and the stage of the cancer. Metastatic kidney cancer generally has a worse prognosis than pure, isolated kidney cell carcinoma.
Renal cell carcinomas that are easily operable and grow in one piece on the surface of the kidney have a particularly good prognosis. If these are surgically removed in good time, a recovery can be assumed. Papillary and chromophobic types are also more often limited to the kidneys (i.e. do not spread) and have a good prognosis.
The more lymph nodes are involved, the worse the prognosis. In the case of metastases, it is generally unfavorable. While a local tumor that is not scattered still has a mean five-year survival rate of 90 percent, if the lymph nodes are involved it is only around 60 to 70 percent. In the case of distant metastases, for example in the brain or the lungs, the figure is only 15 percent.
It should be noted that early detection is still the best influence on a favorable prognosis for renal cell carcinoma. People with risk factors (genetic diseases, kidney weakness, etc.) in particular benefit from check-ups. If a carcinoma eventually develops in the kidney, it can usually be treated quickly.
prevention
Since the exact origin of renal cell carcinoma has not yet been clarified, prevention is difficult. Risk factors such as constant use of painkillers or smoking should be avoided.
Aftercare
A follow-up check or follow-up care is urgently required after every cancer therapy. This is due to the fact that many tumors form again after a while. There is also the risk of metastasis growth, which regularly leads to a shortening of life expectancy.
Follow-up care is usually discussed before the end of the initial therapy. The doctor and patient determine the location and the rhythm. Quarterly follow-up care in the first year is common. The interval then widens from appointment to appointment. From the fifth year onwards, an annual performance is sufficient.
This type of aftercare aims to closely monitor the patient in order to prevent complications from occurring in the first place and to enable diagnosis at an early stage. The latter brings with it the best healing prospects. Follow-up care includes a detailed interview and a physical examination.
A blood test is usually also carried out. Imaging methods such as CT or MRI are used as required. Follow-up care can also be of a palliative nature. Then there is no longer any chance of a cure for renal cell carcinoma. Doctors try to enable the patient to lead a symptom-free life. Medication and assistance in everyday life form an important foundation for this.
You can do that yourself
Pure self-help measures that have a medical or even therapeutic effect on renal cell carcinoma do not exist. There are no home remedies, exercises or other measures that sufferers can usefully take. Rather, it is not advisable to take unpredictable agents and substances experimentally. However, pain management measures can be taken if necessary. It is important that the means used do not burden the kidney.
It can help the patient if he is very well informed about renal cell carcinoma. This type of cancer has been well researched and the information is readily available. Knowing about one's own illness makes treatment and one's own condition more understandable and can accordingly help to overcome fears. It also gives patients more security when talking to doctors if they are well informed themselves.
Since a renal cell carcinoma also stresses the healthy parts of the kidney or kidneys, it is also advisable to design a diet that is kidney-friendly. This means a significant reduction in the amount of salt supplied and an increase in the amount consumed. The amount of salt should be around five grams or less per day, the amount you drink should be increased to around 2.5 to 3 liters. The meat content in the diet can also be reduced in order to further relieve the kidneys.

.jpg)
.jpg)
















.jpg)