Vaginal discharge, vaginal discharge are terms for everyday occurrences of moisture and discharge in the area of the female sexual organs (vagina).
causes
They come from secretions that can take on the most varied of properties: pure white, as it were milky, glassy or glassy-milky, purulent, purulent-slimy, purulent-watery, yellowish, frothy, greenish or reddish. The amount of secretion changes.Sometimes it is only slight, but women often have such strong discharge that they are constantly bothered not only by the feeling of moisture, but also by unpleasant side effects such as soreness, burning, ulceration and pain.
The smell can be bland, slightly sweet or even foul-smelling, even smelly.
It is understandable that women turn to the gynecologist when they see such symptoms in order to be relieved of their complaints. However, help is only possible if the cause of these various types of secretion is sought, if the actual source of the discharge can be determined.
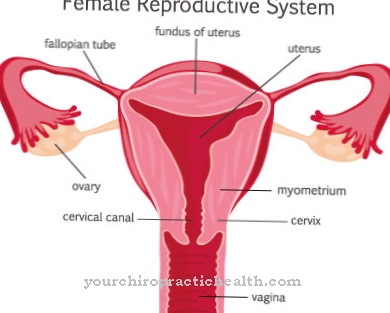
The discharge takes place mainly in the area of the lower genital parts, namely in the cervical canal, in the vagina or vagina and within the atrium of the vagina. But the whole section is not always affected, often only individual parts are the actual causes of discharge and affect the other areas. The main sources of secretion and their likely causes are discussed here.
Symptoms, ailments & signs
Unusual vaginal discharge and itching, combined with a burning sensation in the vaginal area, could be signs of infection or inflammation. Burning when going to the toilet or pain during sex also indicate an unbalanced vaginal flora. Depending on the pathogen, further symptoms occur.
If the vaginal discharge is thin and light gray, bacterial vaginosis is suspected. The vagina feels dry despite the increased discharge. If there is an unpleasant to foul-smelling intimate smell of fish, it is very likely that the vagina is infected by bacteria.
White, crumbly vaginal discharge, paired with severe itching, suggests a fungal infection. With vaginal mycosis (yeast infestation), the discharge usually does not smell. In some cases, however, it can take on a slightly sour odor.
If parasites (trichomonads) are the trigger for the inflammation, yellowish discharge occurs. Sometimes the vaginal secretion is greenish to frothy and has an extremely unpleasant smell. Sometimes pain occurs in the lower abdomen that cannot be precisely assigned.
If the vaginal entrance is infected with vesicles that are very painful, it is probably due to an infection by herpes viruses. If vaginal inflammation is left untreated, the pathogens can spread to the uterus and ovaries and cause other diseases.
Emergence
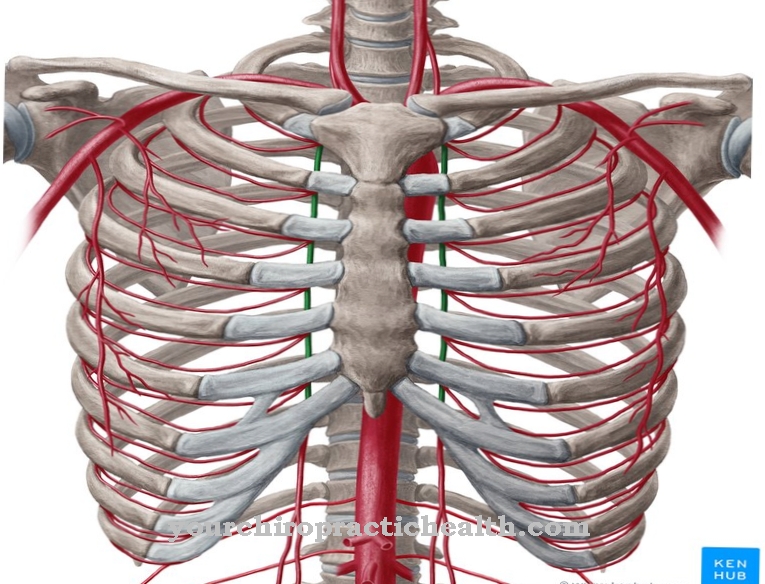
One of the most important sources of leakage is the cervical canal. This canal, about two to three centimeters long, is lined with skin rich in glands, with the number of glands and their dimensions differing from person to person. On the other hand, they are all equipped with a slime-forming top layer. This mucous membrane in the cervix is constantly producing mucus that is closely related to a number of biological processes.
Under normal conditions, the substance flowing out of the cervical canal is not produced in sufficient quantity to create a sensation for the woman of discharge or fluorine, as it is called in technical jargon. However, conditions often develop in the cervix that increase mucus and thus become sources of discharge. The reasons for this are manifold.
These include the formation of scars on the cervix, which are caused by the act of childbirth and when the wounds heal poorly after delivery. Scar strands are formed and the originally tubular, smooth neck canal shows clear tears, so that the delicate glandular mucous membrane is no longer protected.
Similar phenomena occur when the glandular mucous membrane of the cervical canal, whether congenital or as a result of childbirth, occupies the surface of the cervix protruding into the vagina. Even then, the sensitive gland cells are exposed and react - stimulated by the foreign milieu - with increased mucus production. This increased secretion is generally still bearable and remains within certain limits. Only when the exposed, easily vulnerable areas of the mucous membrane become inflamed, does a strong, sometimes purulent discharge become noticeable, which can cause extremely great discomfort.
But even with a completely intact cervical canal, increased mucus secretion can occur. Because apart from chronic irritation of the glands as a result of previous inflammations in the area of the cervix - the glandular tubes are preferred hiding places for all kinds of bacteria - nervous and hormonal causes play a very important role here.
Function of the vagina
The lining of the glands in the neck canal is influenced by the ovarian hormones and the nervous system. Therefore, the cervix can be stimulated to increased secretion both with overactive and underactive ovarian glands and increased nerve excitability, similar to the stomach with nervous mucosal inflammation.
Sensitive, easily excitable women are particularly susceptible to this. There is no doubt that mere sexual ideas and feelings can increase the secretion of mucus, which can be the reason for erotic desires, reading, dreams and films alone. To the same extent, the defense against unwanted partners, sexual conflicts outside and within the marriage and partnership sometimes play a role that should not be underestimated for the increase in mucus and thus for the development of the discharge feeling.
It should also be mentioned that, of course, benign or malignant tumors and swelling, slimy, watery, purulent, but in cancer usually bloody secretions cause. For this reason alone, every woman should consult a gynecologist if discharge occurs, because this is the only way to recognize a cancerous tumor.
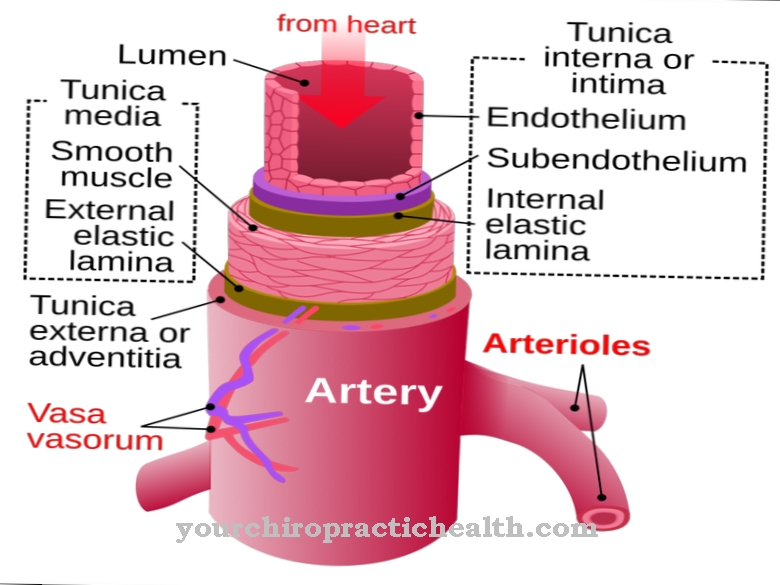
Structure of the vagina

The vagina is a muscle tube, the inner skin of which consists of a thick layer of several layers of flat cells (so-called plaster epithelium) stacked on top of each other. Although there are no secreting glands in the vaginal wall, there is a whitish, often more pasty, sometimes whitish-liquid mass in the clearing that lies against the vaginal wall without causing the sensation of discharge. This substance, which is mainly composed of exfoliated vaginal wall cells and rod bacteria - so-called Döderlein vaginal bacteria - is of great biological importance.
It protects the upper parts of the female sexual organs (uterus, fallopian tubes, abdominal cavity) from the penetration of pathogenic germs from outside. This is done with the help of lactic acid, a relatively strong acid that is formed by the Döderlein bacteria from the sugar present in the flaked cells.
However, this acid protection can be disturbed or even interrupted by various causes. For example, a large amount of alkaline mucus can flow from the cervical canal into the vagina and at the same time weaken the acid that forms. Foreign germs (pus pathogens) can also penetrate the vagina, be it that a poorly closing entrance, as can occur after births, offers no resistance, be it that the bacteria, among other things, with flushing fluids or rings to repair uterine subsidence and Incidents getting into the vagina. Under such conditions, the contents of the vagina multiply and flow out of the vagina more strongly, giving the woman the feeling of discharge.
The more harmless changes in the vagina described so far are opposed to those that are accompanied by vaginal inflammation. The discharge is then usually thin, watery or purulent, sometimes even bloody.
Vaginal Inflammation & Discharge
This discharge, which sometimes smells unpleasant, causes the feeling of sharpness or burning and soils the external genital organs and thus also the underwear. As microscopic examinations have shown, this secretion no longer contains Döderlein bacteria (lactic acid bacteria), but instead a lot of pathogenic pus germs and a large number of white blood cells, which shows that the foreign germs that have penetrated have gained the upper hand and caused inflammation. The vaginal wall is therefore also very reddened, swollen with inflammation and very sensitive to pain.
The causes of this clinical picture are just as varied and often cannot be found out at all. However, it is clear that in any case the activity of the ovaries plays a major role, as it regulates the function of the vaginal wall. Disturbances in the ovaries can therefore - in a negative sense - affect the defense mechanism of the vagina. In addition, of course, all kinds of pus germs and gonococci are important for the development of such a disease.
Small flagellates, so-called trichomonads, and thrush fungi - the same pathogen that often causes white deposits in the mouth of small children - are also considered to cause very persistent and painful vaginal infections. They make themselves particularly uncomfortable through severe itching and burning. The inflammation can develop into ulcers, which of course complicates the treatment.
Not only the internal, but also the external genital organs consisting of folds and bulges, large and small labia, can cause discharge. The skin and mucous membrane glands in the bulges secrete sebum, fat, mucus and sweat and thus protect the tissue from drying out, urine flowing down, etc. These secretions are usually so small that a feeling of moisture does not arise. However, their increase and change also lead to discharge. The sensory nerves of the external genital organs play a major role here, and they are most sensitive to irregular wetting.
More inflammation & eczema of the vagina

It is therefore understandable that slimy or purulent-watery drainage from the upper parts irritates and inflames the delicate and sensitive mucous membrane of the external genitalia. This is especially true for the purulent vaginal inflammation caused by trichomonads and thrush fungi. Understandably, the external urethral opening is also included, which usually leads to pain when urinating. In the case of strong, corrosive discharges, inflammation and eczema can even occur on the neighboring skin and thighs, which considerably complicates the clinical picture.
But the external genitalia can also develop inflammatory disease in isolation, in women of all ages. The possible causes here are uncleanliness, a reduction in resistance in the case of severe general illnesses and chemical or mechanical stimuli.
Finally, the feeling of moisture on the external female genitals is also caused by abnormally strong secretions from the mucous glands there. These glands are heavily influenced by the nervous system, so mood, nervousness or sexual arousal can be blamed for a discharge.
Complications
A vaginal infection with vaginal discharge can cause various complications. If the inflammation spreads to the cervix, it can lead to inflammation of the fallopian tubes and ovaries. This can lead to infertility or an ectopic pregnancy, which can lead to further complications. During sexual intercourse there is a risk of contagion to the partner.
If vaginal inflammation occurs during pregnancy, you may also favor premature labor or premature rupture of the bladder. In the most severe cases, vaginitis leads to a miscarriage. Occasionally, the colpitis pathogen spreads to the child and causes serious health complications in this as a result. The vaginal discharge can cause inflammation and occasionally a urinary tract infection.
It is also accompanied by a strong feeling of discomfort. When treating vaginitis with vaginal discharge, the risks come from the prescribed antibiotics. These can cause various side effects and allergic reactions. Symptoms of the gastrointestinal tract, headaches and body aches, skin irritations and, rarely, damage to the liver and kidneys are typical. Incorrectly used home remedies can also cause problems and under certain circumstances further irritate the vaginal environment.
When should you go to the doctor?
As a rule, vaginal discharge is natural and therefore does not require medical treatment. It is also normal for vaginal discharge to change consistency and intensity over the course of the cycle. However, there is usually a need for action if the secretion suddenly takes on a different color or has a noticeable odor. Some bacterial or fungal infections have the potential to heal spontaneously without medical attention.
If the vaginal secretions turn pink or brown, this may indicate the implantation of an embryo in the uterus, the imminent occurrence of menstruation or ovulation. For this reason, it is sometimes advisable to wait a few days before seeing a doctor. If there is also inflammation or other symptoms such as pain and itching, a specialist should be consulted as soon as possible. Self-treatment is not advisable. In young girls, vaginal discharge first occurs some time before their first period (menarche).
It is a natural process. To be on the safe side, however, this can be clarified with a gynecologist. Not absolutely necessary, but often advisable, is a visit to the doctor in the event of strong or weak vaginal discharge. These complaints are usually not related to illnesses, but the gynecologist can prescribe preparations to alleviate them.
Treatment & Therapy
This multitude of causes makes it impossible to judge the discharge from uniform criteria. This results in the need to research the cause or source of the abnormal outflow substance in each individual case, taking into account the overall personality (emotional life, state of the nervous system, general illnesses) of a person. In most cases, it is possible to identify the cause of the discharge through precise examinations of the external and internal genitals or organs and with the help of microscopic observations of the secretions, which the gynecologist then holds in his hands with the key to its elimination.
From what has been said, it goes without saying that there can be no general remedy for vaginal discharge and that the treatment measures must be different depending on the type or cause of the discharge. In any case, it is important to identify and eliminate the source of the fluorine and to restore the proper functioning of the genital organs and the normal structure of the vaginal wall. As already mentioned, finding the causes is made significantly more difficult, on the one hand by their multitude and on the other hand by the fact that they can lie outside the sexual organs.
Let us only think of general diseases such as cirrhosis of the liver, diabetes, Graves, infectious diseases and pathological nervous conditions, which are also to be regarded as causes of discharge. Of course, all of this complicates the treatment, which always has to be individual and does not allow generalization. Complete success can therefore only be guaranteed if the patient follows all medical instructions and does not lose patience during the usually lengthy treatment.
You can do that yourself
Vaginal discharge and vaginal inflammation are not uncommon problems that can often be managed well with self-help. Precondition is an exact diagnosis by the doctor. Once this has taken place, self-help by the woman can in many cases replace another visit to the doctor if the patient's appearance flares up again. Common to the discharge and the inflammation is usually a bacterial imbalance. The environment that is natural in the vagina can often be easily restored with lactic acid bacteria. There are suppositories or tablets that are inserted into the vagina. Alternatively, a tampon coated with natural yoghurt can be of great help. It also cools the tissue, which is often reddened by the infection. Itching can also often be relieved naturally in this way.
Hygiene is important when it comes to vaginal discharge. But many women overdo it in this context and use harsh detergents to bring the vaginal environment out of harmony even more. Mild cleaning, preferably only with lukewarm water, is sufficient here.In addition, when using the toilet, care should be taken that wiping with the paper is always from the vagina towards the anus and not the other way around. Laundry is best to be washed at high temperatures and of course to be changed daily.

.jpg)







.jpg)
.jpg)
.jpg)







.jpg)