A Vaginal prolapse refers to an outward protrusion of the vagina. He is also called Vaginal prolapse Designates and medically represents a fourth degree vaginal depression.
What is a vaginal prolapse?

A vaginal prolapse is the protrusion of the vagina outward. There is at least one more or less visible leakage of the vaginal mucosa. This exit can be seen in the genital area of the woman. In this way, the vagina expands out of the body and enters between the labia.
Furthermore, the vaginal prolapse can be enlarged by the discharge of further organs. These organs then take up the space that the vagina previously occupied. Whether this happens depends, among other things, on which part of the vagina emerges. For example, the cervix (less often the uterus), the urethra and the bladder can also be affected. The posterior vaginal wall also emerges less frequently, which can lead to rectal involvement.
Vaginal prolapse can also be subdivided, whereby the extent must be determined. A complete vaginal prolapse is known as prolapsus vaginae completus sive totalis, involvement of the cervix as prolapsus vaginae et cervicis. Partial forms, in which the lowering of the internal female genital organs do not lead to a strongly visible prolapse, are accordingly also referred to as prolapsus vaginae incompletus sive partialis.
For the definition, the distinction between a vaginal sagging and a vaginal prolapse is relevant: The vaginal sagging means a change in the localization of the internal organs, while a vaginal prolapse explicitly means the exit. The vaginal sagging has a total of four degrees of severity and the vaginal prolapse represents the fourth degree of vaginal sagging. With the other three degrees, there is no leakage of the organs.
In this context, involvement of the urinary bladder is referred to as a cystocele, involvement of the urethra as a urethrocystocele and involvement of the intestine as a rectocele. Usually this is linked to the degree of the vaginal prolapse. If the lower third is affected, a urethrocystocele is almost inevitable. In two thirds of the cases, the cystocele follows, and if the posterior vaginal wall has loosened, a rectocele can occur. The corresponding organs then enter the unused space and sometimes also displace the components of the vagina.
causes
The causes of a vaginal prolapse are based on the holding apparatus of the vagina and the stress a woman experiences. The holding apparatus itself, which largely consists of ligaments and muscles, is used over the years. Every birth presents a special challenge, especially with large children and multiple births. Accordingly, a vagina rarely fully recovers from a birth process, but is still functional.
A single birth is rarely the cause of a vaginal prolapse. Rather, vaginal births can turn out very differently depending on the health, age and physique of the woman giving birth. Sometimes the vagina itself and the holding apparatus are injured due to overstretching. The so-called maternal ligaments are particularly stressed during births.
Menopause and aging also play a role. The holding apparatus loses its elasticity due to aging and can accordingly favor changes in the position of the internal organs. Almost every woman past menopause also has a slight vaginal sagging. This is normal.
Lifestyle is heavily to blame for the health of the vaginal structures. Overweight, for example, has a counterproductive effect due to the continuously increased pressure. It is the same with chronic constipation and frequent, strong coughs. Improper lifting of heavy loads is also a risk factor for the occurrence of all types of prolapses.
Removal of the uterus (hysterectomy) can also lead to a vaginal prolapse if the vaginal blind sack is not sufficiently attached. It can find its way down due to gravity and exit. Overall, it often happens that the vaginal prolapse only develops gradually and the leakage of the vagina is triggered by a single event and thus becomes visible.
Symptoms, ailments & signs
Signs of an approaching vaginal prolapse are sometimes difficult to determine, as freedom from symptoms is the norm until the actual prolapse. However, changes in the vagina can sometimes be detected through eye inspections.
The vaginal prolapse itself causes few symptoms. A foreign body sensation may occur in the vagina. Most women experience a feeling of pressure or tension that seems to strive downwards. There is also back pain, which can get worse during the day. However, severe pain is rare in this context. The vaginal prolapse is also visible, at the latest after a slight spread of the labia.
In addition, when the bladder and rectum are involved, there are corresponding symptoms in this area. A urethrocele with a cystocele can lead to incontinence, a long-range cystocele, however, can lead to urinary retention and a rectocele can impede defecation.
Complications
The complications in connection with a vaginal prolapse arise primarily from the organs involved. Sometimes it is no longer possible to reverse the vaginal prolapse without surgical measures. This carries the usual risks of surgery. In this context, the uterus is often removed, which naturally prevents fertility.
At most, urinary retention can still be dangerous. After a certain period of time, this can affect the kidneys, which can ultimately lead to life-threatening sepsis if the bladder is not relieved.
When should you go to the doctor?
A vaginal prolapse will usually move affected women to the doctor quickly. The strong change in the genital organs can be felt and seen.
In addition, a vaginal prolapse cannot usually be corrected manually by the person affected. Going to the gynecologist is recommended here. If urinary retention has occurred, an emergency department should also be visited so that the bladder can be relieved quickly and the kidneys are not affected.
Overall, every vaginal prolapse is worth assessing and requires treatment. While in some animal species such a vaginal prolapse occasionally occurs and this also reverses itself, this is rarely the case with humans.
diagnosis
The diagnosis is made primarily through an external examination of the vagina. The doctor can quickly determine whether it is a whole vaginal prolapse or a persistent vaginal sagging. The vaginal prolapse is easier to spot. Once the diagnosis has been made, the lower abdomen is also checked (for example using ultrasound) in order to check for any possible displacement of other organs.
Part of the diagnosis also consists of an anamnesis in which the patient and doctor work through moments that could have led to the prolapse. This is relevant to pinpoint the exact cause of the vaginal prolapse. This results in specific instructions for follow-up care after treatment.
Treatment & Therapy
Treatment of a vaginal prolapse consists of acute treatment and follow-up care. The aim of acute treatment is to return the vagina to its original state. Operative and non-operative procedures come into consideration. The non-operative procedure essentially consists of using pessaries. These objects are inserted into the vagina and are primarily used to support the uterus. So they are mainly used when the uterus has passed through the vagina.
A pessary can consist of different materials and be shaped very differently. It is intended for long-term use. Otherwise, operative procedures must be mentioned, all of which are considered uncomplicated.
The vagina can be tightened (on the front or back wall), with the cervix often being surgically changed or removed. This procedure is often used for a common vaginal prolapse. If the uterus is also partially or fully involved, a hysterectomy is preferable.
Should organs have penetrated into the resulting space as a result of the incident, they will be manually repositioned. Sometimes an attachment of the organs is necessary, which is often done through small incisions through the abdominal wall. Aftercare essentially consists of pelvic floor muscle training and avoiding certain activities.
Outlook & forecast
The prognosis for a vaginal prolapse is considered to be favorable. Almost all incidents of this type can be resolved in a satisfactory manner. Sometimes the insertion of a pessary is sufficient. The women who have experienced a vaginal prolapse do not have to fear any restrictions with regard to sensations in the sexual area.
Vaginal prolapses also have no effect on births and pregnancies unless the uterus is removed. It should be noted, however, that a woman can experience more than one vaginal prolapse. This depends very much on the integrity of your internal support system.
prevention
The vaginal prolapse can be prevented indirectly. The measures listed here serve to keep the vagina and the structures that support it healthy. In this respect, it makes sense to simply not do certain things or to do them rarely. When lifting heavy loads, for example, you should not lift from your back, but from your knees. This lifting technique results in a straight back, which means less pressure on the vagina.
Endurance sports, such as swimming or cycling, help overall to strengthen the internal and external muscles. However, pelvic floor muscle training is the best preventative measure. Here you can specifically influence the holding behavior and the feeling of tension in the vaginal area. Not only does it increase mindfulness and self-control: it also strengthens the holding apparatus of the vagina.
The pelvic floor muscle training is a preventive measure as well as a measure for aftercare. Obesity should also be reduced. Anyone who has already had a vaginal prolapse should refrain from excessive exercise of the abdominal muscles. Under unfavorable circumstances this can increase the pressure on the vagina.
Aftercare
After the operation, it is advisable for the patient to avoid lifting heavy loads. It is also advisable to strengthen the pelvic floor muscles through continuous pelvic floor training. This has a targeted effect on the holding behavior and the tension in the vagina area. The correct learning of the pelvic floor training should ideally take place under physiotherapeutic guidance and be practiced daily.
It is therefore a preventive and a follow-up measure at the same time. Regular exercise, for example cycling or swimming, is helpful in order to improve general physical fitness and avoid a new vaginal prolapse. Excessive exercise of the abdominal muscles should, however, be avoided as this may increase the pressure on the vagina.
Since severe obesity, chronic constipation and chronic cough also pose risks, these factors should be counteracted as part of follow-up care. A successfully treated vaginal prolapse usually has no further health consequences. Unless the uterus has been removed, it has no effect on further pregnancies and births.
Sex life is usually not restricted after the healing phase is complete. However, a lack of follow-up care increases the risk of having another vaginal prolapse.
You can do that yourself
In the event of a vaginal prolapse, there are hardly any possibilities for self-help that can change the optical conditions. Close cooperation with a doctor is therefore necessary for this disorder.
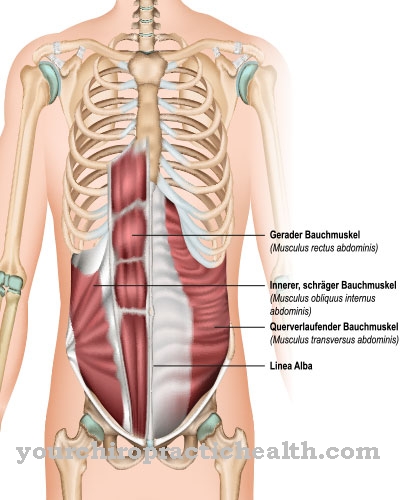
Various techniques can be used to manage the condition that improve general wellbeing. Targeted training of the muscles in the pelvic floor area can help to tighten the muscles and thereby alleviate the symptoms. The abdominal wall solidifies through certain regular training sessions and improves the health of those affected. The exercises can be learned and carried out independently or together in a physiotherapy treatment.
If a surgical procedure is carried out, sufficient rest should take place. In addition, a balanced diet is recommended for optimal wound healing. Sexual practices should be tailored to the needs of the organism. However, it is not advisable to completely renounce physical closeness, as these studies show that these studies generally support well-being and quality of life.
In order to avoid complications and side effects, the use of non-prescribed medication for pain relief should be avoided. Cognitive training can help in coping with the pain, as can the use of various natural remedies. A sufficient supply of heat to the abdomen enables many sufferers to reduce the symptoms that have occurred.


.jpg)
















.jpg)