Schizoaffective Disorders are mental illnesses that manifest themselves either in one phase or in alternating phases in manic, depressive and schizophrenic symptoms. Melancholic depressive symptoms are just as much a part of the clinical picture as manic high spirits and schizophrenic catatonic, paranoid or hallucinatory phenomena
What is schizoaffective disorder?

© yamasan - stock.adobe.com
The concept of schizoaffective disorder is a collective term for mental illnesses that simultaneously or alternately contain the symptoms of depression, schizophrenia and mania. Schizoaffective disorders thus stand between schizophrenia and affect psychoses, with their symptoms primarily resulting from the overlap between these two areas.
According to ICD-10, the patient must have affective and schizophrenic symptoms in the same phase for a diagnosis of a schizoaffective disorder. This means that mental illnesses in this direction are not actually individual illnesses, but rather variably concentrated combinations of three different mental illnesses.
The weighting of the symptoms can vary. Schizoaffective disorders were described for the first time in the middle of the 19th century, when mixed psychoses or incidents were mentioned. It was not until the first third of the 20th century that the term schizoaffective illness became established.
causes
So far, medicine has assumed a causal genetic factor for schizoaffective disorders, but this has not yet been determined. Neurochemical and neuroendocrinological, the clinical picture has not yet been further researched.
Mental and psychosocial factors such as stress, privately or professionally stressful situations, environmental reactions as well as partnership, family and friendship difficulties are likely to develop into an additional influencing factor on the onset and course of the disease. A certain personality structure with increased susceptibility to this form of mental illness has not yet been determined.
Symptoms, ailments & signs
A major symptomatic area of schizoaffective disorder are melancholic-depressive symptoms such as sleep disorders, feelings of guilt, or thoughts of suicide. On the other hand, manic symptoms such as considerable arousal, excessive irritability or an enormous increase in self-propulsion can also make up the main symptomatic area.
In addition to these symptoms, there are those of schizophrenic disorder, which manifest themselves in catatonic, paranoid, or hallucinatory properties. In addition to an affective disorder according to ICD-10, the patient also suffers either from an ego disorder such as the expression of thoughts, from a control mania such as the delusional influence, from commenting or dialogizing voices, from a persistent and completely unrealistic delusion, from confused language or from catatonic symptoms such as negativism.
The most common symptoms in the early phase include a tired, dull and quickly exhausted or moody and slightly aggressive mood. Mood swings between cheerful, resigned and depressed are just as common. In addition, anxious-phobic signs of illness can occur. In addition, there are often memory and concentration disorders or increasing forgetfulness, decline in performance and restless and nervous tension.
Often there is also pain for no apparent cause. Changes in behavior are conceivable and are usually expressed in mistrust and social withdrawal. In addition to increased sensitivity to noise and light, abnormal and hardly comprehensible discomforts can occur.
Diagnosis & course of disease
The diagnosis of a schizoaffective disorder is made according to ICD-10. Schizoaffective psychoses are either phased-recurrent or single-phased. In the single-phase course, a distinction is made between schizodepressive, schizomaniac and bipolar disorders. The phase-revising course occurs more frequently than the single-phase course form.
In this case, the individual phases can each correspond to a schizophrenic illness episode, a purely depressive illness episode, a purely manic illness episode, but also a mixed manic-depressive illness episode. On the other hand, the individual phases can also consistently be mixed manic-depressive, schizodepressive, schizomaniac or bipolar. In individual cases, the symptoms consistently of a schizophrenic and mixed manic-depressive illness, i.e. the illness manifests itself in schizomaniac-depressive episodes.
Complications
Even if the episodes build up one after the other, this can happen under certain circumstances without intermediate intervals of complete health. Almost all schizoaffective disorders show several types of progression at the latest in the late course, which means that the symptoms often change. Overall, only a third of the patients remain stable. A more favorable prognosis is associated with more schizomaniac episodes than with more schizodepressive forms. The schizodepressive form in particular tends to become chronic later on.
Due to these disorders, those affected suffer from a significantly reduced quality of life and severe restrictions in their everyday life. As a rule, the disease leads to a number of different psychological complaints. Those affected suffer from severe sleep disorders and thus also from depression or psychological disorders. The feeling of permanent excitement can also occur and make everyday life difficult.
Most patients appear irritated or slightly aggressive. Furthermore, it can lead to paranoid feelings or hallucinations, which can have a very negative effect on social contacts. Those affected often suffer from an obsession with control and strong mood swings. Especially in children, the disease can significantly limit and delay the development of the child.
The children also suffer from disorders of concentration and often appear restless or nervous. The disease can also lead to a strong sensitivity to noise or light and continue to complicate the patient's everyday life. This condition is usually treated with the help of medication.
However, antidepressants can be responsible for various side effects. It cannot be predicted whether the treatment will lead to a positive course of the disease. The life expectancy itself is usually not reduced or restricted by the disease.
When should you go to the doctor?
A doctor is required in the event of abnormal behavior or emotional distress. Insomnia, hallucinations or delusions should be examined and treated. If there are mood swings, memory problems or a very nervous appearance, a doctor should be consulted.
If there is a marked change in drive or behavior that is self-endangering or puts other people in a dangerous situation, you should consult a doctor. A lack of sensitivity to illness is characteristic of schizoaffective disorders. Therefore, the relatives or people from the social environment have a special responsibility.
In the case of a stable and healthy relationship of trust, you should aim to see a doctor together with the person concerned so that a diagnosis and medical care are made possible. In particularly severe cases, a medical officer must be called. If social rules are disregarded, if there is activity or if the person concerned becomes indifferent, he needs help.
Sensory sensitivity, hearing voices, or communicating with imaginary beings are symptoms of the disorder. A visit to the doctor is required as actions are often performed based on the delusions that are hurtful. If everyday life can no longer be managed without help or if severe fears are evident, a doctor is also required.
Treatment & Therapy
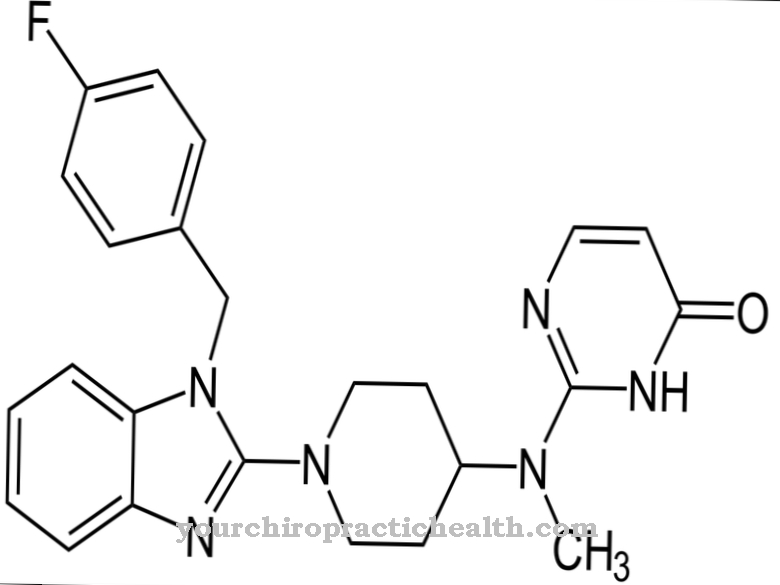
In the acute stage, the therapy and treatment of schizoaffectively disturbed patients is based on the prevailing symptoms. Treatment with neuroleptics is indicated for predominantly schizophrenic symptoms, while lithium can also be used against predominantly manic symptoms. Antidepressants can be given medically against predominantly depressive syndromes, whereby waking therapy is often indicated for psychotherapy.
In addition to acute treatment, patients with a schizoaffective form of the disease also receive phase prophylaxis, which can focus on carbamazepine or lithium, for example. Depending on the individual case, a two-pronged phase prophylaxis may also be necessary, which combines the drugs mentioned with neuroleptics. The accompanying psychotherapy focuses on current conflicts and stressful situations. The focus here is on coping with the disease and dealing with the consequences of the disease.
You can find your medication here
➔ Medicines to calm down and strengthen nervesprevention
In view of the presumably mainly genetic risk factors of schizoaffective disorders, the disease can hardly be prevented. Anyone who recognizes the symptoms of the early course mentioned above can at least benefit from an early diagnosis by contacting a specialist.
With a schizoaffective disorder, the person concerned suffers from schizophrenia and also from manic or depressive moods. In severe cases, he is affected by all three disorders alternately.
Aftercare
As with all mental illnesses, aftercare is a necessary part of therapy. Avoiding relapse is the ultimate goal. If the person concerned takes psychotropic drugs against the symptoms, the psychotherapist controls the healing process. If the disorder has been treated satisfactorily in this way, close follow-up care is no longer necessary.
Occasional appointments for follow-up checks should still be arranged. The type of aftercare depends on the severity of the symptoms and the question of which mood fluctuations besides schizophrenia burden the patient. Parallel depressive traits require a different aftercare than manic disorders.
A schizoaffective disorder can lead to incapacity for work if the disease is severe. This brings with it the risk of additional depression. During the aftercare, the sick person is built up and a possible feeling of worthlessness should be taken away. A schizophrenic with shopping addiction as an expression of mania runs the risk of falling into debt.
You can also intervene at follow-up appointments here. Sometimes a debt advisor has to be called in for this. Close relatives often experience the disease as a burden. In such situations, follow-up care extends to the patient's parents or relatives in order to better manage the disease and its effects.
You can do that yourself
In the case of a schizoaffective disorder, the options for self-help are extremely limited. Because of the disorder and the associated impairments, the person affected can do little to improve his own situation. He is dependent on the help and support of other people in the long term. Only relatives and members of the social environment can have a positive influence on further developments through their behavior, understanding and decisions. Cooperation with a doctor is essential for this disease.
In addition, it is extremely beneficial for the well-being of the person concerned if a stable social environment is available and maintained over the long term. Although this illness usually involves an inpatient stay, regular contact with relatives is supportive and helpful in coping with the illness. According to studies, the feeling of security and a regular daily routine have a positive influence on the patient. The intensity of the complaints is demonstrably lower when there is continuous contact with trusted and family members. Joint activities that are tailored to the needs of the sick person help to improve the overall situation.
In addition, influencing factors such as a healthy diet and the avoidance of harmful substances such as alcohol or nicotine are advisable.

.jpg)







.jpg)
.jpg)
.jpg)







.jpg)