A Pain pump enables patients to independently administer a specific dose of pain medication. The process known as 'patient-controlled analgesia' is used by pain and palliative medicine specialists as part of a specific therapy.
What is a pain pump?

A patient-controlled pain pump continuously supplies the body with medication. The small electronic device is used for severe, chronic pain. Medicine has relied on this form of treatment since the 1980s, especially after serious surgical interventions. In addition to clinical use for pain treatment (analgesia), it helps patients with long-term medication at home.
The application of painkillers, tailored to individual needs, using the PCA (Patient-Controlled Analgesia) takes place at the push of a button and without the intervention of nursing staff or a doctor. She regularly releases a set amount of the pain reliever (analgesic) via the vein or directly into the spinal cord. There it reaches the required high effective level, also known as a bolus, quickly and immediately. In individual cases, if necessary - controlled by those affected - an additional, technically limited dose can be called up.
External models wear people attached to their bodies. For long-term therapy, a surgeon places the palm-sized pump under the skin with a simple operation.
Shapes, types & types
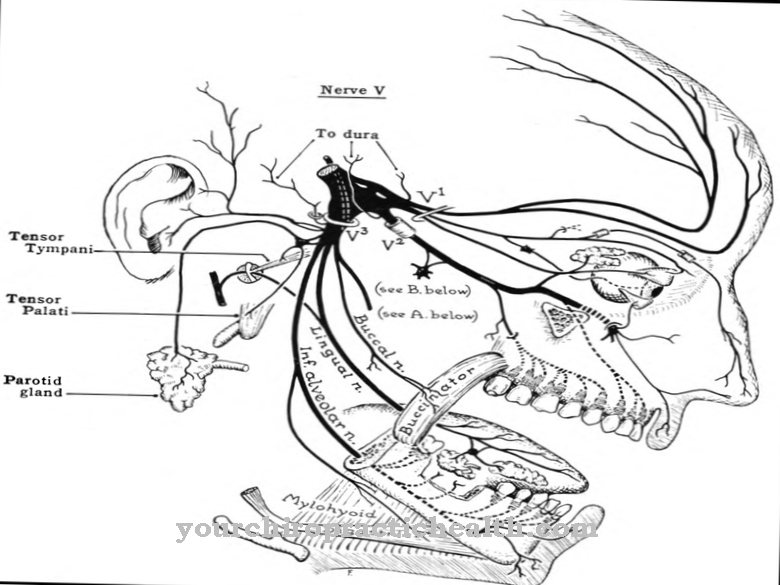
A distinction must be made between intravenous, intrathecal and non-invasive transdermal pain pumps. In the majority of cases, the former remain outside the body and transport the medication by means of a tube. It enters the subcutaneous fatty tissue through a needle. Alternatively, the attending physician creates direct access to the vein via a port (intravenous PCA).
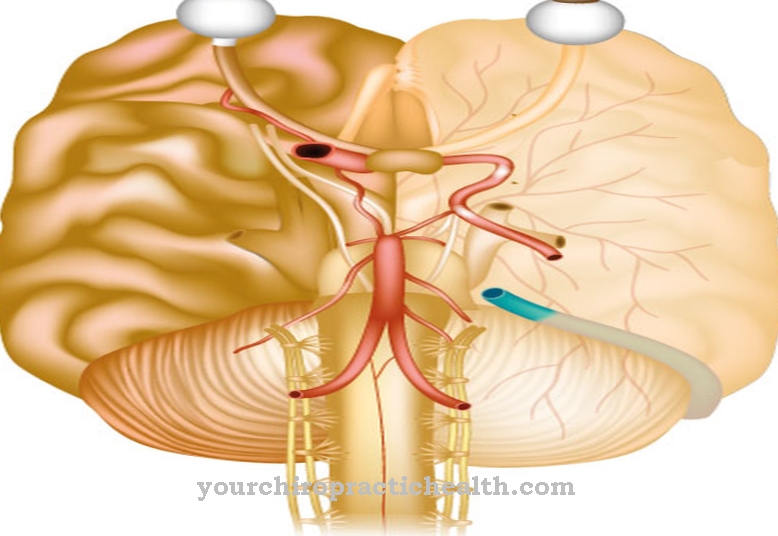
The size of the devices depends on the volume of the necessary storage container. As a rule, this refillable reservoir holds between 20 and 40 milliliters. In the intrathecal pain pump for patient-controlled epidural analgesia (PCEA), a catheter guides the pain reliever to the spinal cord or into the spinal canal.
Patient-controlled regional anesthesia (PCRA) works in a similar way for a peripheral nerve block - only the location varies. An example of application is the baclofen pump, which is used to treat spastic pain in injuries to the spinal cord and in multiple sclerosis.
The non-invasive transdermal PCA is another physical procedure. The attached electronic system administers the active ingredient, an opioid, at the push of a button using a weak direct current through the surface of the skin.
Structure & functionality
The basic structure of pain pumps is comparable. They consist of different technical components. This includes a lockable reservoir for the pharmaceuticals, the infusion line and a power supply unit, a battery or a rechargeable battery. By pressing the bolus button, the pump injects the analgesic and slowly releases it through a thin tube into the connected system.
The delivery quantity and blocking intervals - periods in which the electronics do not allow any further bolus - is controlled by a programmable microprocessor. It stores and transmits infusion and usage logs via a connection to a PC. The evaluation helps the anesthetists to optimize the therapy plans.
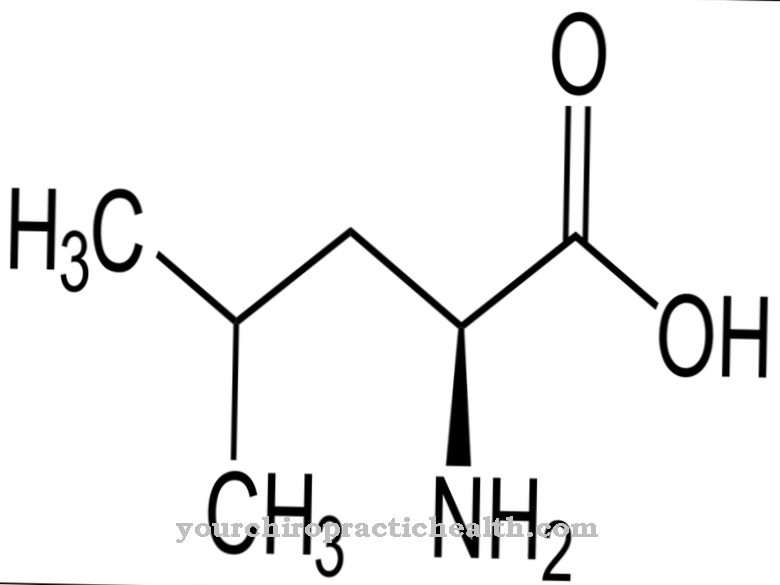
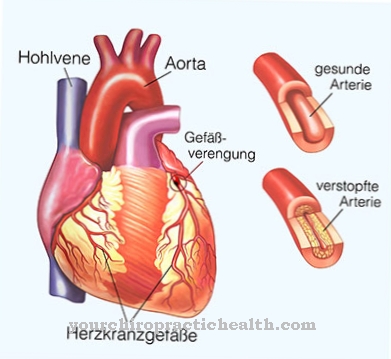
The pain relievers used are mainly opioids such as morphine, fentanyl or sufentanil. In addition, medicine uses the ziconotide and local anesthetics originally obtained from the venom of the cone snail.
The patient-controlled pain pumps should be refilled regularly. Depending on the size of the storage container, the amount to be injected and the frequency, this takes place at intervals of a few weeks to a few months. In the case of implanted pumps, the doctor does the filling with an injection. The implantation of a PCA requires chronic pain that cannot be treated with other measures or only with significant side effects. The surgeon normally places the pain pump below the costal arch in the upper abdomen after placing a catheter to the spinal cord.
You can find your medication here
➔ Medicines for painMedical & health benefits
Doctors mainly use a pain pump after operations and for chronic pain syndromes. Other important areas are tumor therapy and palliative medicine.
One of the decisive advantages of pain therapy using PCA is its high degree of effectiveness. The specialist determines the amount of pain reliever by determining the bolus through tests. At the same time, a blocking interval prevents unconscious or deliberate overdosing. The administration of opioids leads to a short-term decrease in consciousness (vigilance). It is not possible to administer further medication to yourself at this stage.
Patient-controlled analgesia often provides those affected with self-determined, rapid relief from acute pain. The supply is reliable and the side effects remain limited. The procedure also relieves the gastrointestinal tract. For patients, it means fewer restrictions and complaints and, as a result, a higher quality of life. It makes everyday life easier, especially in the case of cancer-related symptoms.
Before a PCA is indicated, intensive examinations under inpatient conditions are necessary. Understanding of the affected person for the treatment method is crucial for success and uncomplicated use. Psychologists and pain therapists check whether the pain pump is suitable or whether alternative methods can be considered.
For example, allergies and intolerance to opioids, depression, severe sleep disorders or cognitive deficits should be excluded. Further contraindications exist in the case of adhesions on the spine, blood clotting disorders and disorders of consciousness. Continuous medical checks are carried out for the safety and protection of the sick. Patient-controlled analgesia is one of the most efficient options for pain therapy.







.jpg)