Spondylosis refers to a number of problems with the spine caused by wear and tear on the intervertebral discs. Physiotherapy, pain medication, or surgery can help alleviate symptoms of wear and tear. Most people over 65 have some form of spondylosis.
What is spondylosis?

© bilderzwerg - stock.adobe.com
Spondylosis is a general term for problems with the intervertebral discs of the spine, which usually arise with increasing age.
When the intervertebral discs dehydrate and shrink, bone spurs and other signs of osteoarthritis develop. Spondylosis is very common and gets worse with age. It is believed that a genetic component is also to blame, as some families have more cases of spondylosis than others.
However, more than 90 percent of people over 65 will develop some degree of spondylosis, which can be seen on x-rays. However, many people do not notice any serious symptoms of spondylosis. If these occur anyway, conservative treatment is usually successful.
causes
In the course of life, the physics of the human spine changes due to various loads that can lead to spondylosis. The intervertebral discs act as a kind of buffer between the vertebrae.
Most people begin to shrink and dehydrate their intervertebral discs from the age of 40. This leads to increased bone contact and discomfort. Discs that are weakening can also be damaged, which often leads to nerve irritation.
The weakening of the intervertebral discs can also lead to a misdirected reaction of the body, which results in increased bone growth. These bone spurs interfere with the normal movement of the spine. Ligaments between the vertebrae can also stiffen with age and restrict freedom of movement, which is also a common sign of spondylosis.
Symptoms, ailments & signs
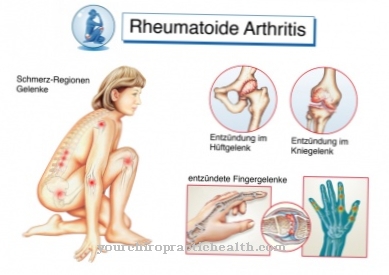
Spondylosis can manifest itself through a number of symptoms and complaints. The disease manifests itself, among other things, in severe pain in the neck, spine, buttocks and legs. The complaints occur in individual places or in the entire back area and sometimes radiate to the buttocks.
Accompanying this, tensions can occur, which are usually perceived by the sick as extremely stressful. Those affected describe the pain as throbbing to stabbing. In addition, there is an unpleasant tingling sensation. Symptoms appear when you move and decrease when you rest. As the disease progresses, the pain gradually decreases.
However, there may be limitations in the mobility of the spine in the long term. Those affected are then no longer able to lean their upper body forward or to the side. Movements such as bending over or lifting are associated with severe pain. If the course is severe, there may be permanent restrictions on movement. In principle, however, spondylosis can be treated well, and chronic complaints are rare. The disease is usually over within a few weeks to months.
Diagnosis & course
For a diagnosis of Spondylosis the doctor will usually begin with a physical exam. The focus is on the mobility of the spine and whether certain movements trigger pain or tension.
The strength and reflexes of the muscles are also checked here. This is usually followed by one or more imaging procedures. Simple x-rays of the neck can show whether displacements or bone spurs have developed that cause poor posture, pressure or pain. A computed tomography offers the possibility to depict the spine from many different angles and also to show minor damage.
Magnetic resonance imaging (MRI) can also show changes in the soft tissue of ligaments or help pinpoint areas where nerves are being squeezed. For a myelogram, a liquid is injected into the spine before the x-ray that is more clearly visible on the images. But an electromyogram can also show the effects of a possible spondylosis more precisely. The latter test measures the activity of the nerves.
Complications
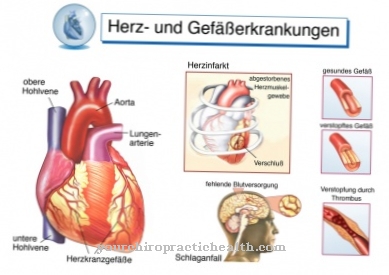
Spondylosis can, among other things, favor hernias in the spine. A typical complication of the disease is what is known as osteochondrosis. This disease can also be traced back to wear and tear of the intervertebral discs and occurs more frequently in the context of spondylosis. Chronic neck and back pain can also occur.
Complaints in the lumbar spine and intervertebral discs cannot be ruled out. Long-term illnesses can cause painful muscle tension and paralysis. This leads to general movement restrictions and, depending on which treatment method is chosen, adverse events can occur. With drug therapy, a decrease in mental and physical performance is possible.
In addition, side effects and interactions as well as allergic reactions can occur. An injection with prednisone carries similar risks, but can also lead to infections at the injection site and other symptoms. An undetected heart disease can cause cardiovascular problems and, in the worst case, even cardiac death. Surgical intervention also carries risks.
Occasionally there are nerve injuries and the resulting sensitivity disorders and temporary symptoms of paralysis. Scars can develop after the operation or unpleasant wound healing disorders occur.
When should you go to the doctor?
Since spondylosis does not heal on its own, the person affected should always consult a doctor with this disease. The earlier the doctor is consulted and the treatment started, the better the further course is usually also. Therefore, the patient should contact a doctor at the first symptoms and signs of spondylosis. A doctor should be consulted if the person concerned has severe pain in the neck or back. Even severe restrictions in movement can indicate spondylosis and should also be examined by a doctor if they occur over a long period of time.
Many people also suffer from tingling sensations in various parts of the body or from severe numbness. Furthermore, tension or severe pain in the muscles can indicate spondylosis and must also be examined by a doctor. The first diagnosis can be made by an orthopedic surgeon or a general practitioner. For further treatment, treatment by a specialist is usually necessary.
Treatment & Therapy
Treatment of Spondylosis depends on the signs and symptoms. The goals of treatment are to limit discomfort and pain, maintain normal activity, and prevent further damage to the spine.
If common painkillers no longer help, the doctor may prescribe muscle relaxants. These help if regular back cramps occur. In some cases, drugs that are otherwise used to treat epilepsy have also proven helpful. They act on the damaged nerves. Stronger narcotics may be needed to manage more pain. An injection of prednisone into the affected areas has also proven to be a promising therapy.
Treatment for spondylosis can be done with a physical therapist. This teaches exercises that help those affected to strengthen weak areas of the back and relieve others. This often leads to a reduction in symptoms. When all conventional treatments fail, surgery is the only option. This ensures that there is enough space again for intervertebral discs and nerves.
You can find your medication here
➔ Medicines for back painprevention
The Spondylosis is a result of wear and tear. High stress on the back from repetitive physical activity over a long period of time can lead to premature spondylosis. An increased body weight is also a risk factor and leads to back problems more quickly. The same applies to permanent incorrect posture and insufficient movement of the back muscles. Accordingly, attention should be paid to diet and health sports.
Aftercare
The treatment strategies of aftercare in patients with spondylosis are primarily aimed at the pain symptoms. The pain treatments can be done through the use of medication or through local anesthesia procedures. Alternative procedures in aftercare include acupuncture and psychological pain therapy and behavioral therapy.
In addition, by learning relaxation techniques, the patient can contribute to their own pain relief. Examples include progressive muscle relaxation, autogenic training and yoga. As part of the aftercare, the doctor advises the patient and explains the prognosis, the coping strategies for everyday activities and encourages the patient in a targeted manner.
It is about the primary task, the balancing act between protecting the patient in phases of pain and activating and avoiding longer phases of relaxation. Sports therapy measures are not advisable in acute periods for patients with spondylosis. On the other hand, light gymnastic exercises can help reduce pain and counteract immobility.
Complex movements are thus preserved and restored. In addition, physiotherapy and occupational therapy can be used in acute phases. Through conservative treatments, it is quite possible to achieve pain relief in the affected areas of the patient's movement.
You can do that yourself
In the case of spondylosis, rest and rest. The affected joints are very painful and often swell up.This can lead to restricted mobility, which may also pose a health risk. Therefore, those affected should spend the first days and weeks after diagnosis in bed.
In order to avoid sores and other complaints, however, care should be taken to exercise gently. A daily walk or 15 minutes of physiotherapy help alleviate the symptoms. It may take a few days for the prescribed pain relievers and anti-inflammatories to take full effect. Which measures are necessary in detail for a spondylosis depends on the individual course of the disease. In the case of slight complaints, rest and relaxation are sufficient.
Since spondylosis is a degenerative disease, there are no long-term treatment options. The patients often need therapeutic support, for which a psychologist or a specialist therapist is responsible. If conservative treatment is no longer effective, surgery is necessary. After this, bed rest is important. The wound must be carefully cared for to avoid inflammation and infection. Depending on the symptoms, the doctor will prescribe further medication.


.jpg)

















.jpg)



