The Theca cell is a type of connective tissue and occurs in the ovarian follicle, where it plays an important role in follicular maturation. Under the influence of LH, the cells become thekalutein cells by luteinization, as they are in the corpus luteum. Theca cell tumors and granulosa-theca cell tumors are the most well-known diseases of the tissue type and count among the hormone-forming tumors.
What is the theca cell?
Ovarian follicles consist of an egg cell and the surrounding follicular epithelial cells, also known as granulosa cells. The unit also contains the connective tissue layers theca interna and externa, which are summarized as theca folliculi. Maturing ovarian follicles consist of different types of cells.
One type of cell in the ovarian follicle is the so-called theca cell, as it is found in the theca folliculi and plays a major role in the growth of the follicle. The thekalutein cell is to be distinguished from the theca cell. These cells occur exclusively in the corpus luteum and develop from theca cells of the ovarian follicle. Counter cells are thus the preliminary stage of the counter cells. Luteinization in the sense of the storage of lipids differentiates more mature thekalutein cells from conventional theca cells.
Anatomy & structure
Theca cells are a variant of connective tissue found only in the ovarian follicle. Histologically, mobile and local cells form the connective tissue in extracellular collagen matrices or amorphous basic substance. Extracellular matrices form a three-dimensional meshwork with proteoglycans within the spaces.
The tough cell-fiber structure makes connective tissue almost resistant to tensile forces and the basic substance distributes compression forces. The theca cells are differentiated connective tissue which, in the form of theca folliculi, surrounds the ovarian cortex zone (cortex ovarii) like a seam and envelops the ovarian follicle in the later stage of maturity. In contrast to undifferentiated connective tissue, the specialized and differentiated theca cells are capable of storing and producing substances. Thekalutein cells contain stored lipids, for example.
Function & tasks
Theca cells take on different functions during the maturation of the ovarian follicle. They support the growth and final maturation of the female follicle by expressing membrane-bound LH receptors. These receptors represent a binding site for the luteinizing hormone. The peptide is synthesized in the adenohypophysis and stimulates the secretion and synthesis of estrogens in the female gonads.
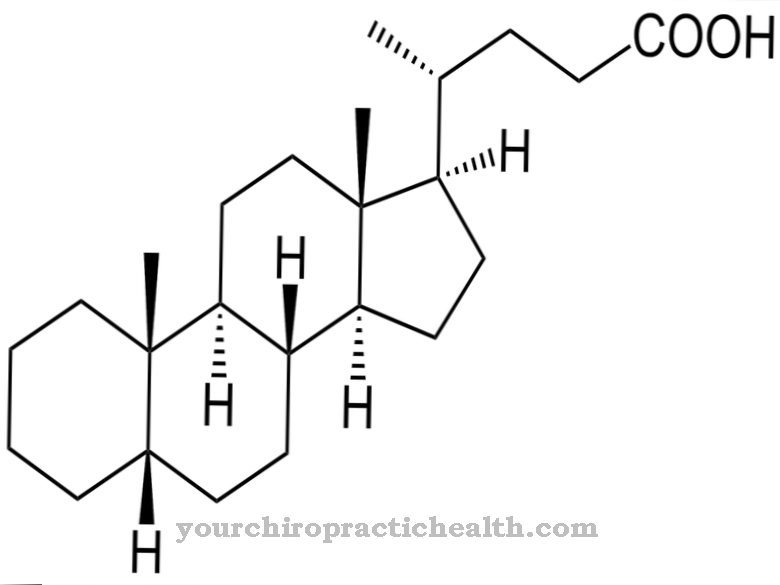
LH is a dominant regulatory factor in the second half of the female cycle. In the first half of the cycle, the hormone stimulates the synthesis of estrogens, with the release increasing sharply towards the middle of the cycle. This LH surge triggers ovulation, i.e. ovulation, and stimulates the synthesis of the corpus luteum. With the binding of LH to the LH receptors within the theca cells, the synthesis of steroids is triggered. More precisely, the complex formation causes the production of testosterone. Under the influence of FSH, the testosterone is converted into the estrogen variant estradiol within the granulosa cells of the follicles.
In addition, theca cells luteinize to form thekalutein cells as found in the corpus luteum. The influence of LH causes hypertrophy in the theca cells, which leads to the storage of lipids and turns the theca cells of the ovarian follicle into thecalutein cells of the corpus luteum. Basically, the formation of theca cells goes hand in hand with the development from the primary follicle to the secondary follicle.
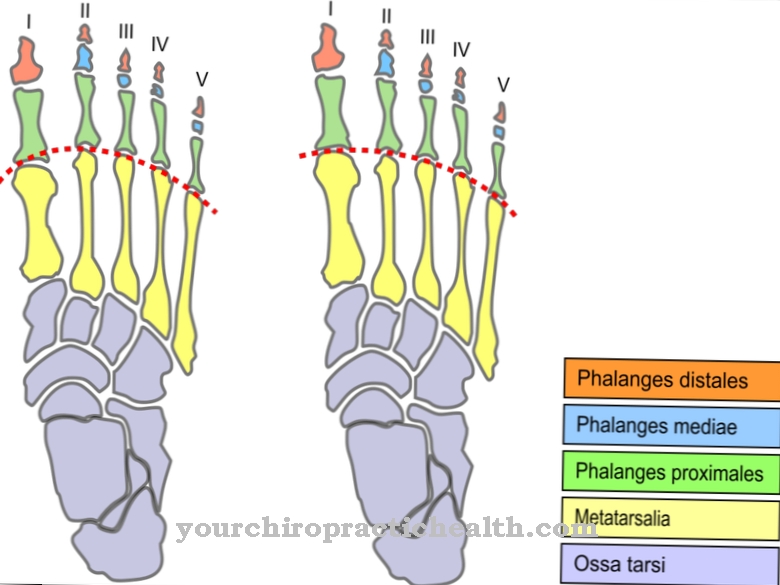
The stage of the tertiary follicle causes the cells to differentiate into functionally and histologically different cell layers. In this way, theca interna and theca externa of the ovarian follicle develop. The inner cell layer Theca interna, like the granulosa cells, is responsible for the estrogen synthesis in the follicle. The theca externa consists of contractile cells that drive the egg from the mature follicle during ovulation.
Diseases
Ovarian tumors are among the hormone-producing tumors and can originate from different types of tissue in the ovary. In addition to granulosa cell tumors, there are, for example, theca cell tumors. Mixed forms are known as granulosa-theca cell tumors. The tumors from these types of tissue produce estrogens and, in some cases, androgens and occur more frequently in women between the ages of 50 and 60 years.
The mixed form of granulosa cell and theca cell tumors is also known as the luteinizing variant of ovarian tumors and is particularly evident in women between 20 and 30 years of age. The type of tissue of the tumors allows a prognosis. Apparently, the likelihood of malignancy is related to the type of cell. Granulosa cell tumors, for example, are malignant in up to 50 percent of all cases. Theca cell tumors, on the other hand, only have a probability of around twelve percent. This means that in most cases pure theca cell tumors are benign tumors of the ovary.
According to various sources, the luteinized variant of granulosa-theca cell tumors is benign in almost all cases, whereas the conventional granulosa-theca cell tumor is malignant with a probability of up to 27 percent. The symptoms of ovarian tumors from degenerate theca cells differ mainly with the age of the patients. Postmenopausal women often experience bleeding as the first symptom. Pre-puberty girls often develop isosexual precocious puberty. This means that their sexual characteristics are fully developed before puberty.
In this case, the symptoms also partly affect the skeleton. The development of symptoms for the theca cell tumor and the granulosa-theca cell variant depends primarily on the hormones formed by the tumor and the level of hormone production. In addition to estrogens and androgens, the tumors can also produce other hormones in individual cases, which can then be detected in higher concentrations and can bring the entire organism out of balance.



.jpg)






.jpg)

.jpg)
.jpg)











.jpg)