The term thyrotoxic crisis describes a sudden and life-threatening metabolic imbalance. It usually develops on the basis of an existing overactive thyroid.
What is a thyrotoxic crisis?

© bilderzwerg - stock.adobe.com
The thyrotoxic crisis is a life-threatening derailment of an overactive thyroid gland (hyperthyroidism). The clinical picture develops within a few hours or days. In the thyrotoxic crisis, all symptoms of hyperthyroidism are very pronounced.
The crisis is often triggered by an increased iodine intake or an x-ray contrast medium containing iodine. The thyrotoxic crisis occurs about one to four weeks after admission. Stopping anti-thyroid drugs can also cause a thyrotoxic crisis. The crisis requires immediate intensive care. If left untreated, it can lead to death.
causes
A thyrotoxic crisis can only develop from an overactive thyroid. If you have an overactive thyroid, the thyroid gland produces too many thyroid hormones. The two most important thyroid hormones are triiodothyronine (T3) and thyroxine (T4). The basic component of the thyroid hormones is the trace element iodine. The main cause of the overactive thyroid is the autoimmune disease Graves' disease.
The body's own antibodies bind to the TSH receptors of the thyroid gland and thus mimic the effect of the thyroid-stimulating hormone (TSH) from the pituitary gland. This leads to a constant production of T3 and T4 and thus to an overactive thyroid. An overactive thyroid can also develop as a result of thyroid autonomy. With thyroid autonomy, individual areas of the thyroid work independently of the hormonal regulatory mechanisms.
Furthermore, hyperthyroidism can be caused by hormone-producing tumors of the thyroid gland and by thyroid inflammation. The thyrotoxic crisis usually develops after a high iodine intake. This means that the body has more iodine available for the production of thyroid hormones. Since the body's own hormonal regulatory mechanisms are disrupted in the case of an overactive thyroid, production is not contained.
The thyrotoxic crisis is often iatrogenically induced, i.e. by the doctor, by administering drugs containing iodine. X-ray contrast media are also frequent triggers. It also becomes dangerous when patients with an overactive thyroid stop their medication on their own.Anti-thyroid drugs stop the thyroid gland from making too many hormones.
Suddenly stopping the medication can result in a thyrotoxic crisis. Surgery can also cause a thyrotoxic crisis. In particular, after thyroid tissue has been removed, the thyroid's hormone production can reactively increase.
Symptoms, ailments & signs
Typical symptoms of an overactive thyroid include insomnia, irritability, and nervousness. In many patients a subtle tremor, a slight tremor, can be observed as a sign of restlessness. The entire metabolism is stimulated by the thyroid hormones. The blood pressure is high.
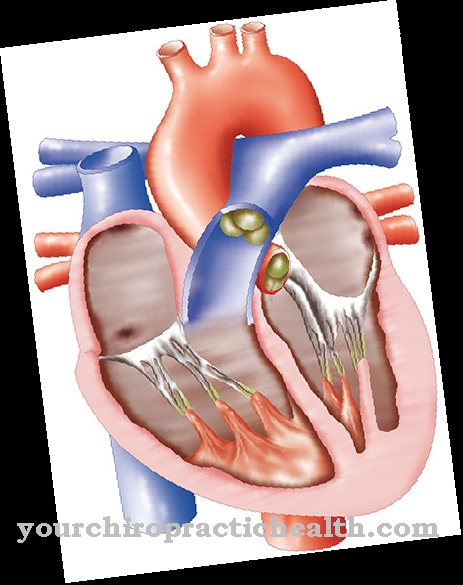
The difference between the systolic and diastolic blood pressure values (blood pressure amplitude) is increased. The heart's activity is changed. The heart beats faster, and some suffer from heart stumbling (extrasystoles). Atrial fibrillation can also be the result of hyperthyroidism. The patients are hungry due to the increased energy expenditure, but still lose weight.
Due to the mobilization of glycogen reserves and fat reserves, hypoglycaemia (hyperglycaemia) can occur. Patients sweat quickly, are heat intolerant and have moist, warm skin. You have to use the toilet more often and have thin stools. The muscles are weak. In the thyrotoxic crisis, all these symptoms intensify massively and within a very short time.
In stage I of the thyrotoxic crisis, the heart rate is increased to more than 150 beats per minute. Patients vomit and have a high fever. Desiccosis can develop due to the increased fluid excretion. In stage II of the crisis, patients are increasingly disoriented and clouded in consciousness. You are drowsy or sleepy. In stage III, the sick fall into a coma.
The increased heart rate, cardiac arrhythmias and dehydration are particularly threatening. If left untreated, the coma threatens irreversible long-term consequences. Overall, the prognosis for the thyrotoxic crisis is rather poor. It often ends fatally.
Diagnosis & course of disease
A suspected diagnosis can be made quite quickly based on the characteristic symptoms. An already known hyperthyroidism provides the decisive clue. The increased thyroid values can be detected in the blood during the thyrotoxic crisis. The TSH value is very low.
TSH stimulates the thyroid gland to produce thyroid hormones. Since there are far too many thyroid hormones in the blood due to the thyrotoxic crisis, the pituitary gland produces less TSH. The values of the thyroid hormones T3 and T4 are nevertheless increased.
Complications
If a thyrotoxic crisis sets in, this affects the entire metabolism. The blood pressure is increased, there is nervousness, irritability and sleep disorders, and tremors occur. In addition, the heart's activity is changed and those affected suffer from heart stumbling and atrial fibrillation - both of which can lead to serious complications up to and including heart failure.
In addition to the general symptoms, there is weight loss, which is usually associated with dehydration and deficiency symptoms. The mobilization of glycogen and fat reserves can lead to hypoglycaemia. In addition, the patients are physically ailing and suffer from muscle weakness. In the thyrotoxic crisis, all of these symptoms increase within a very short time. High fever, dehydration and impaired consciousness occur relatively quickly.
Then the patients fall into a coma. A loss of consciousness in the absence of treatment or treatment that is too late usually has irreversible long-term consequences or even leads to death. The treatment of a thyrotoxic crisis can be affected by the typical side effects and interactions of prescribed drugs. Surgical intervention is always risky, as the patient is usually already considerably weakened.
When should you go to the doctor?
High blood pressure, internal restlessness, nervousness and irritability are complaints that should always be clarified by a doctor. If they persist for several weeks or months, they must be examined. If the irregularities increase, a doctor's visit is necessary immediately. If there are disturbances in the heart rhythm, a decrease in muscle strength or a loss of general resilience, it is advisable to consult a doctor. Fever, vomiting, malaise and a feeling of illness should be presented to a doctor. Since the thyrotoxic crisis is a health emergency, acute changes in well-being often occur within a short period of time.
In the event of sudden discrepancies, an emergency service should be alerted. A characteristic of the disorder is that those affected lose weight in advance, although they consume an unusually high number of calories every day. Unwanted weight loss is the body's alarm signal. In the event of disorders of consciousness, disorientation or memory disorders, an ambulance service must be called. People present are obliged to use first aid measures. Without timely and professional medical care, the affected person threatens a comatose state and irreparable damage to organs. Therefore, there is an urgent need for action if there is a significant deterioration in health.
Treatment & Therapy
The thyrotoxic crisis is always treated in the intensive care unit. The functions of the cardiovascular system are closely monitored. In addition, the fluid supply and fluid excretion are monitored. In this way, the fluid can be balanced and desiccosis can be counteracted. Those affected receive three to four liters of fluids per day. Furthermore, drugs are used that limit the production and release of thyroid hormones.
These include anti-thyroid drugs such as thiamazole and glucocorticoids such as prednisolone. Beta blockers regulate the increased heart rate. If the fever is severe, ice packs can be used for cooling. Paracetamol or ibuprofen can also lower the fever. Sedation can be used if the patient is very agitated.
If the thyrotoxic crisis was triggered by an iodine contamination and none of the measures described help, the thyroid gland is almost completely removed in a surgical procedure. Plasmapheresis can also be done to remove the iodine from the blood.
prevention
Consistent treatment of the overactive thyroid can usually prevent a thyrotoxic crisis. Patients with known hyperthyroidism should not take drugs that are high in iodine. Thyroid function should also be checked in special situations, such as infections or operations.
Aftercare
In contrast to an overactive thyroid, the thyrotoxic crisis poses an acute danger to life. It does not develop chronically, but takes on a brilliant course. As a rule, however, the crisis is preceded by an overactive thyroid. Timely medical intervention is necessary to prevent a life-threatening outcome of the disease.
In such cases, treatment and aftercare run in parallel. The aim of the therapy is to normalize the thyroid values and to avert the life-threatening condition. The danger to life is not the same with every thyrotoxic crisis. In the early stages, a fatal outcome is around 10 percent likely, in the advanced stages the probability is already 30 percent.
The last option in severe cases is surgical reduction of the thyroid gland. However, immediate treatment is always necessary. The patient is admitted to hospital for this purpose. When the appropriate medicine is given, the responsible internist checks the healing. In addition, the person concerned receives medication for other complaints such as nausea or dizziness.
If the crisis has been successfully contained, follow-up care is gradually discontinued and ends with the discharge. The usual follow-up methods are scheduled for a thyroid operation. The family doctor carries out occasional follow-up checks. The patient has to keep the appointments so that possible new changes in the thyroid gland can be recognized early.
You can do that yourself
The thyrotoxic crisis is a medical emergency because the patient's health deteriorates rapidly and can possibly lead to death. It is therefore of the utmost importance that patients do not try to alleviate their condition on their own through self-help measures. This is not possible and increases the risk of dying as a result of the thyrotoxic crisis.
If people notice symptoms of a thyrotoxic crisis in themselves or experience other severe complaints, they immediately contact an emergency doctor. Once under medical treatment, patients with a thyrotoxic crisis follow all instructions from staff, whether they are doctors or nurses.
People with a thyrotoxic crisis usually first come to a clinic and are treated as inpatients until their state of health has improved. For this purpose, the patients receive appropriate medication in the prescribed dose. It is essential to take these medicines regularly and properly, otherwise the symptoms may recur. Digestive complaints are also treated with medication, and patients in the hospital are given adequate meals. Since many of those affected suffer from nervousness, sedatives are sometimes used.


.jpg)






.jpg)



.jpg)










.jpg)
