With the transcutaneous vagus nerve stimulation (t-VNS) are used to treat drug-resistant epilepsy and depression. In the area of the auricle, a branch of the vagus nerve is activated with electrical impulses through the skin without the need for an operation.
What is Transcutaneous Vagus Nerve Stimulation?
Transcutaneous vagus nerve stimulation is an alternative to conventional VNS, which involves surgery in the chest area. A pacemaker-like stimulation device is implanted, which is connected to the vagus nerve by means of an electrode.
The stimulation apparatus is connected to the ear electrode by a thin cable. It regularly sends electrical impulses to the brain, which then releases anticonvulsant and antidepressant agents. The device signals are usually broadcast for 30 seconds every five minutes. If the battery in the pacemaker device runs out, it must be replaced in another neurosurgical procedure. With this method, the frequency of epileptic seizures could be reduced by three quarters over two years of use. However, side effects such as cough, hoarseness and voice disorders (dysphonia) occur here. They make themselves felt when the device is working, but wear off over time.
The not inconsiderable consequential effects are due to the stimuli to which the efferent nerve fibers leading to the internal organs are exposed. Various studies have shown that the patients tolerate the transcutaneous VNS well, that it fits into their everyday life relatively easily and that it contributes to an improved general living situation. However, it has not yet reached the therapeutic effectiveness of invasive VNS. The t-VNS can be used for all forms and degrees of severity of the impairments to be treated.
Function, effect & goals
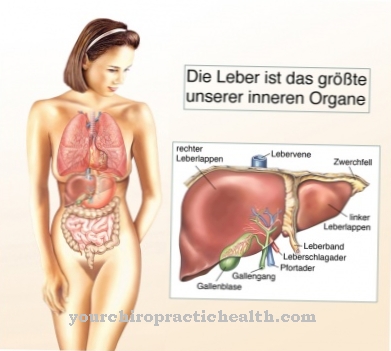
The vagus nerve is one of twelve cranial nerves and drives internal organs such as the heart and lungs as well as the digestive tract. It has an exceptionally large area of distribution in the human body, to which it ultimately owes its name. The Latin word vagari means to roam in German. The stimulating apparatus for the vagus nerve is about the size of a smartphone.
The electrical stimuli are transmitted through the skin to the ramus auricularis nervi vagi (vagus nerve RANV) through a special ear electrode that is worn like small headphones. This branch can excite the vagus nerve and thus transmit signals via the brain stem to the upper areas of the brain, which are said to have an impact-reducing effect. One test found that around 23 out of 100 people with epilepsy had fewer seizures this way. In some subjects, the epileptic seizures even disappeared completely. With such a device, each patient can carry out the therapy himself once a day at any location. The strength of the electrical stimulation can be regulated. A slight tingling or pulsing sensation is usually felt at the point where the device was used.
Remarkable successes have already been achieved with this technique against severe migraine attacks. Initial practical examinations also reveal the chances of recovery from anxiety disorders, Alzheimer's and one-sided headache. In another method of non-invasive transcutaneous vagus nerve stimulation, an electric field is built up at the level of the carotid artery. The vagus nerve can then be stimulated for two minutes by putting on an apparatus the size of a hand. This method is already allowed in Europe for the treatment of anxiety disorders, depression, epilepsy and primary headaches.
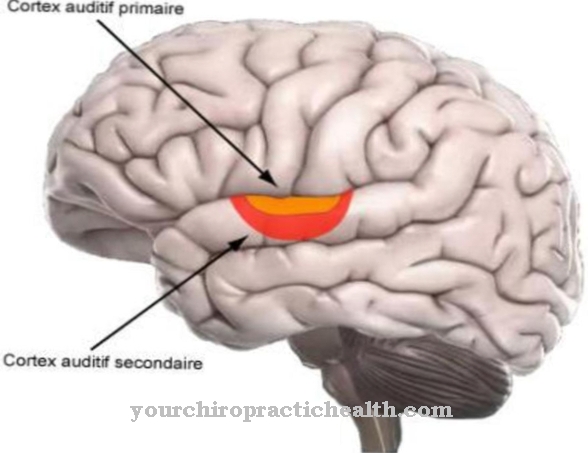
Tests with functional magnetic resonance tomography have shown that transcutaneous vagus nerve stimulation is used to address precisely those areas of the brain as in a surgical procedure. Both methods act on a certain bundle of nerves in the brain stem, which plays an essential role in the development and frequency of epileptic seizures. Around a third of all epilepsy sufferers do not experience any improvement in their condition when they are given relaxing (convulsive) drugs. This situation has not changed significantly in the past few years, despite multiple changes in resources and research.
The stimulating methods are therefore gaining in importance for drug-resistant patients. The risks are considered to be very low, especially in comparison to surgical interventions in which part of the brain tissue is removed in order to reduce the epileptic seizures. Implanting electrodes in the brain is also a relatively risky procedure.
Risks, side effects & dangers
In contrast to invasive methods, transcutaneous vagus nerve stimulation does not cause any undesirable irritation of nerve fibers. This also eliminates side effects such as hoarseness or temporary shortness of breath. Itching or slight pain can only occur in the area of the auricle during stimulation, but these can be minimized or completely eliminated by reducing the intensity of the electrical stimulation.
With the optimal setting of the stimulation strength of his device, the patient only feels a slight tingling sensation in the ear. The sensible daily workload for stimulating the vagus nerve is four hours, which can also be spread over the day. The owner of the stimulation device can change the strength of the electrical stimuli at any time so that it always corresponds best to his own sense of well-being. The patient regularly receives all important information about the effectiveness and duration of the therapeutic measures from the display of the device.
All data is continuously saved in the device so that the attending physician can follow the course of therapy at any time and influence it effectively. The measure can be canceled at any time. Even in children who suffer from epilepsy seizures, t-VNS treatment can be used in combination with medicinal products.











.jpg)





.jpg)