Ulcer molle (Chancroid), also colloquially soft chancre called, is a sexually transmitted disease caused by the bacterium Haemophilus ducreyi. The sexually transmitted disease leads to ulcers on the genitals, accompanied by swelling of the lymph nodes. Ulcus molle can be successfully treated with antibiotics.
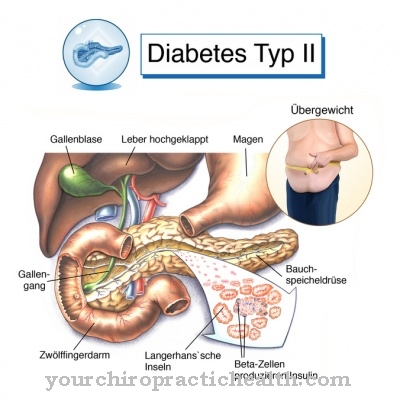
What is ulcus molle?
Ulcer molle is a sexually transmitted infectious disease. The disease is predominantly found in warmer countries and occurs only sporadically in Europe, usually in people who have recently returned from endemic areas.
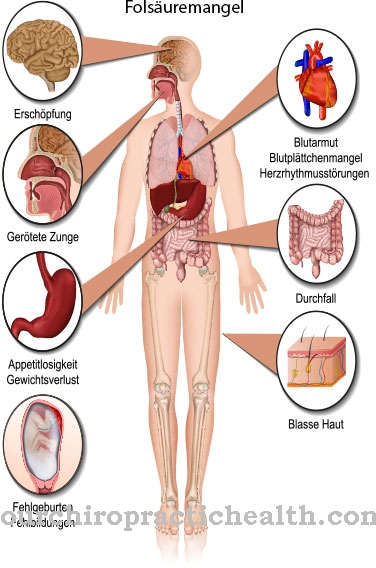
Recent reports from South-East Asia and Africa show that the incidence of ulcus molle in relation to genital herpes is currently falling. Various studies have now shown that ulcus molle is a significant co-factor in the transmission of the immunodeficiency virus type 1 (HIV-1).
The improved diagnosis and treatment of ulcus molle therefore also plays an essential role in combating the HIV-1 epidemic. Mainly men are affected by ulcus molle, while in women the course of the disease in about half of the infections runs without recognizable symptoms.
causes
Ulcer molle is caused by the Streptobacillus Haemophilus ducreyi, which is transmitted through sexual intercourse with infected people. The bacterium is very sensitive to dehydration and cold, which is why it mainly occurs in tropical countries (Africa, Latin America or Asia).
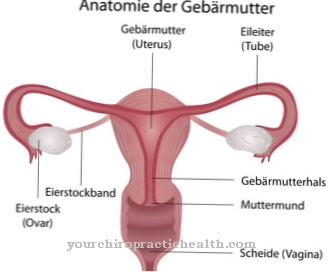
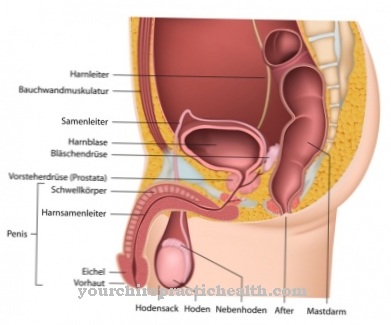
The infectious process of ulcus molle affects the genital skin as a result of tiny epidermal abrasions during sexual intercourse, during which the pathogen lodges under the skin. Initially, slightly inflamed blisters develop 4-7 days after infection before pustules form. Ulcus molle lesions usually occur on the foreskin and penile shaft of men and on the vulva, cervix, or labia of women.
Symptoms, ailments & signs
Ulcus molle is characterized by ulcers in the genital area. Both men and women can be affected. The disease begins with the formation of a small nodule at the point of entry of the pathogen. In the further course, the small lump develops into an ulcer. The ulcer appears irregularly limited, flat and red-rimmed.
It causes severe pain and forms foci of pus that can burst. The edge of the ulcer is soft (lat. Mollis). The soft chancre usually consists of several ulcers that can fuse together. In men, the ulcers mainly show up on the penis, under the foreskin or on the ligament of skin located below the glans.
In women, the ulcers usually appear on the vagina. Since they often do not cause pain there, ulcus molle can also go unnoticed in women. Depending on the practices of sexual intercourse, ulceration of the anus or the oral mucosa is also possible. Half of the patients develop other symptoms that can be traced back to the pathogen spreading via the lymphatic system.
In the groin area it can lead to painful [[inflammation of the lymph nodes inflammation of the lymph nodes. They then swell and can also form ulcers and abscesses. The soft chancre is easy to treat. During the infection, however, the risk of contracting other sexually transmitted diseases is greatly increased.
Diagnosis & course
If the pustules are not treated, flat, painful ulcers with nodular clusters of cells and purulent discharge will form within 2-3 days. Also included Ulcer molle Numerous positive T lymphocytes ulcers, which further increases the susceptibility of HIV-infected people.
The complications of ulcus molle in men include narrowing of the foreskin and progressive ulceration. In addition, there are painfully swollen lymph nodes that can spontaneously break open if there is severe suppuration. A timely diagnosis of ulcus molle is usually only possible with pathological changes. A urologist should therefore be consulted with the first symptoms.
A clinical examination of a smear for the causative agent of ulcus molle from an ulcer or the lymphatic fluid is carried out for diagnosis. In order to rule out an infection with another sexually transmitted disease, the diagnosis is additionally secured by culturing from the pathogen strain. In principle, an HIV test should be carried out in parallel with the diagnosis of ulcus molle.
Complications
In ulcus molle, patients primarily suffer from severe inflammation. This occurs mainly at the point where the pathogen occurred. The area itself is clearly reddened and can also be affected by itching.
Furthermore, a very painful ulcer also forms there due to the ulcus molles, which significantly reduces and restricts the quality of life of the person concerned. In many cases, they also suffer from inferiority complexes or from a reduced self-esteem, as the complaint can also have a very negative effect on the aesthetics of the person concerned. Furthermore, the patient's lymph nodes swell significantly and the person concerned feels weak and exhausted.
The disease can also lead to a painful narrowing of the foreskin. In most cases, ulcus molle can be treated relatively easily and quickly with the help of medication. After about a week, the symptoms disappear and there are no further complications. However, the patients are dependent on regular checks and examinations by the doctor so that there are no further complaints. The life expectancy of the patient is not negatively affected by successful treatment.
When should you go to the doctor?
A doctor should always be consulted with ulcer molle. It is a serious disease that can lead to serious complications if not treated properly. Therefore, with this disease, a doctor must be consulted at the first signs and symptoms in order to prevent further complications or complaints.
The earlier a doctor is consulted with this disease, the better the further course of the disease is usually. A doctor should be contacted if a very severe fever develops. As a rule, the patients feel tired and exhausted and can no longer actively participate in everyday life. A doctor should be consulted if these symptoms occur, especially after unprotected sexual intercourse. There is also severe pain in the joints and general weakness.
The Krnakehit ulcus molle can be detected in a hospital or by a general practitioner.The earlier the doctor is consulted, the better the further course is usually also.
Treatment & Therapy
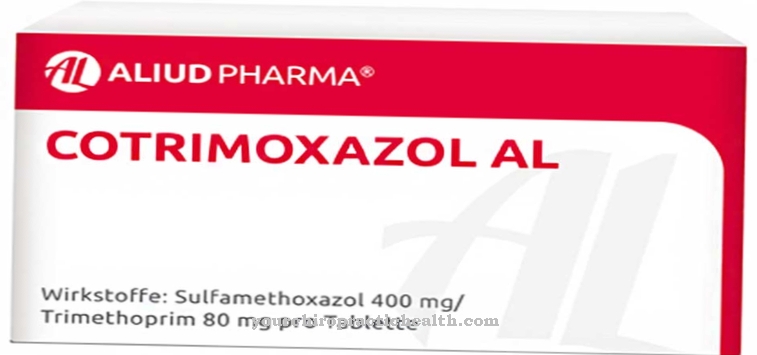
Treatment of Ulcer molle is usually done with antibiotic therapy, and pregnant women should be treated with care. A three-day oral therapy with 500 mg ciprofloxacin twice a day has usually proven effective in the treatment of ulcus molle.
It is also possible to take erythromycin for a period of 7-10 days. Ceftriaxone can also be administered as a single dose intramuscular injection. If necessary, filled lymph nodes are opened in order to anticipate a later inflammatory rupture of the nodes.
In addition, thorough personal hygiene in the genital area is recommended for ulcus molle in order to dry the ulcers or to keep them clean and thus counteract further inflammatory processes. Baths with chinosol, potassium permanganate or anti-inflammatory substances are suitable for this. In addition to the necessity of absolute sexual abstinence, successful therapy also includes the regular sexual partner (s) in the treatment in order to avoid repeated infection with ulcus molle. A follow-up examination after 3 months can confirm healing, thus excluding a chronic condition.
prevention
Basically recommended to avoid infection with Ulcer molle protected sexual intercourse (safer sex). Avoiding the penetration of vaginal or seminal fluid into the body is ensured by using a condom. This is the only way to prevent the pathogen bacterium from entering the body via the mucous membranes.
Aftercare
Medical follow-up care is not necessary if the ulcer molle is completely cured. With early and consistent therapy with antibiotics, it can be assumed that the infection will not have any serious long-term effects. The ulcers heal after a while. Sexual intercourse should be avoided until it has completely healed, so that the weakened tissue can recover and further risks of infection can be excluded. Wearing loose-fitting underwear can facilitate the healing of the affected parts of the body.
Follow-up care may only be necessary for ulcus molle if the bacterial infection has been dragged on for some time. This is especially true if the lymph nodes are already severely affected and purulent abscesses have formed. On the one hand, these need to be opened by the doctor and, on the other hand, represent a gateway for pathogens. In these cases, good wound care is important even after antibiosis.
In cases that are difficult to treat or have been dragged on for a long time, a follow-up examination should also be considered. This can determine whether antibiotic therapy against the soft chancre was completely successful or not. Nevertheless, ulcus molle usually does not lead to serious complications or secondary diseases. Medical follow-up care is therefore not necessary in most cases.
You can do that yourself
An important contribution to self-help in the event of infection with the Haemophilus ducreyi bacterium is to ensure thorough cleanliness and hygiene in the genital area. It is important to keep the ulcers caused by the infection dry and clean to speed healing. In this way, those affected also prevent secondary infections.
It is best to clean the intimate area in the shower. But hip baths with anti-inflammatory substances such as potassium permanganate can also be helpful. Baths with highly concentrated salt from the Black Sea are also said to have a beneficial effect. Salt baths can be painful with open ulcers, so this form of therapy is not recommended for pain-sensitive patients.
It is also important to abstain from sexual activity until the symptoms have subsided. A steady sexual partner should also be included in the therapy, as otherwise there is a risk of permanent mutual infection.
Ulcus molle is usually treated with antibiotics. Women who are sensitive to these active ingredients should use lactic acid suppositories from the pharmacy as a precaution. These preparations stabilize the vaginal environment and can thus prevent treatment with antibiotics from leading to a yeast infection.
In order to prevent new infections, unprotected sexual intercourse should be avoided after successful therapy. In particular, direct contact with vaginal and seminal fluid should be avoided.


.jpg)








.jpg)
.jpg)


.jpg)