As Urogenital tuberculosis is called a tuberculosis of the genitourinary system. This is neither a sexually transmitted disease nor a primary tuberculous disease. Rather, urogenital tuberculosis is one of several possible secondary forms of tuberculosis.
What is Urogenital Tuberculosis?
The Urogenital tuberculosis is a form of secondary tuberculosis in which the organs of the genitourinary system are affected. It usually develops as a result of a primary tuberculosis infection of the lungs.
Although urogenital tuberculosis is not a sexually transmitted disease, the disease must be reported by name. In the countries of Central Europe, urogenital tuberculosis can only be observed very rarely. Most of the diseases occur in two age groups. These are 25 to 40 year old patients on the one hand and elderly patients on the other hand, especially residents of old people's homes.
In Germany too, only relatively few cases of urogenital tuberculosis are observed. In 2006, for example, 1,091 cases of tuberculosis were recorded nationwide in which organs outside the lungs were affected (extrapulmonary tuberculosis). Of these, however, only 27 cases or 2.5 percent were tuberculosis of the genitourinary system.
causes
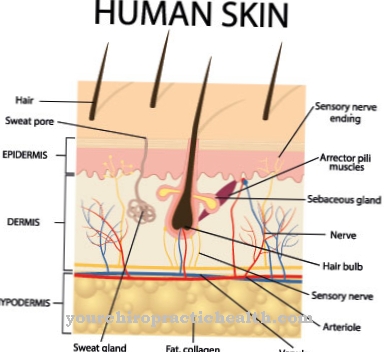
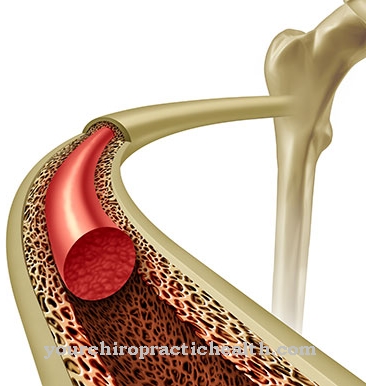
Tuberculosis initially manifests itself elsewhere; often the so-called primary focus is in the lungs. As the disease progresses, however, the tuberculosis pathogens can also affect other organs, to which they usually reach via the bloodstream.
As a result, secondary or organ tuberculosis can develop. If the kidneys, the adrenal glands, the lower urinary tract and the urinary bladder or the genital organs are affected by such a spread of tuberculosis pathogens from the primary focus, urogenital tuberculosis develops.
Typical symptoms & signs
- mostly symptom-free
- Pain and burning sensation when urinating
- Flank pain
- Blood in the urine
- constipation
- Flatulence
- Intermenstrual bleeding or menstrual cycle disorders in women
Diagnosis & course
About twenty percent of the diseases Urogenital tuberculosis cause no discomfort to the affected patient. If symptoms do occur, they tend to be uncharacteristic, such as discomfort when urinating, flank and other pain, pyuria or blood in the urine, as well as flatulence and constipation.
Bleeding disorders or lack of menstruation have also been observed in women. If the man's epididymis is affected, painful swelling and reddening can develop. Various methods are used to diagnose urogenital tuberculosis. The tuberculin test plays an important role here, but is not conclusive and must therefore be combined with other diagnostic methods.
A chest x-ray is used to determine if the patient has primary tuberculosis of the lungs. Further diagnostic procedures are the cultural detection of Tbc pathogens in the urine, which takes about four weeks, the polymerase chain reaction (PCR) for pathogen detection in urine, urography, laparoscopy and the pathogen detection in histological specimens using polymerase chain reaction (PCR ).
In female patients with suspected urogenital tuberculosis, there is also the option of detecting the pathogen in the menstrual blood or a biopsy of the uterine lining.
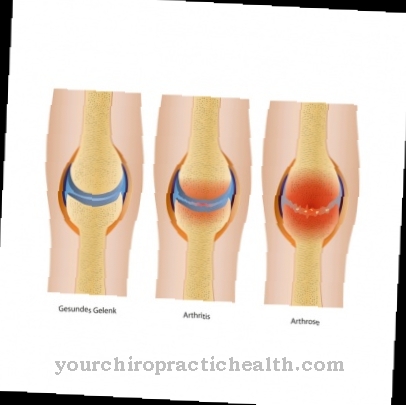
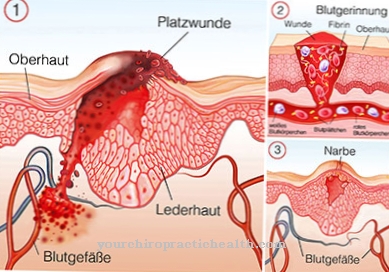
At the onset of urogenital tuberculosis, so-called minimal lesions arise in the tissue of the kidney or other urogenital organs. As a result, a caseating tuberculoma forms, which over time develops into a calcified area. The further course of the disease depends largely on the immune situation of the affected patient.
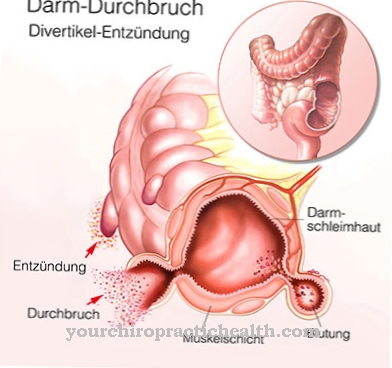
As the urogenital tuberculosis progresses, central tissue deposits (necrosis) and calcifications in the kidney increase. The close juxtaposition of necrotizing areas and the cavity system in the kidney favors the development of deformities. For example, calyx caverns, kidney calyxes, papillary necrosis, but also calyx neck stenoses or narrowing of the renal pelvis can form. The terminal stage of kidney tuberculosis is the so-called putty kidney.
At this stage the organ consists almost entirely of casing necrosis and has completely lost its function. If, as a result of urogenital tuberculosis, scarring forms in the ureters, this can lead to urinary congestion and, in the worst case, hydronephrosis, which can then also lead to a loss of function of the affected kidney.
In addition to the problems described in the kidney and urinary tract, urogenital tuberculosis can also manifest itself in the female or male genitals. In women, the fallopian tube mucous membrane is almost always affected on both sides and the infection spreads into the uterus. When the infection reaches the uterine cavity, it often leads to infertility.
In developing countries such as Bangladesh and India, urogenital tuberculosis is one of the most common causes of infertility in women, and in earlier years tuberculosis of the female genitals was often found incidentally in the course of sterility diagnostics. In men, tuberculosis pathogens can reach the epididymis via the bloodstream, sometimes without involving the kidneys.
The pathogens can also spread to the testes and prostate via the seminal ducts. If tuberculosis affects the genital organs, it must be expected that the disease will lead to infertility in around nine out of ten cases.
Complications
Urogenital tuberculosis does not have to lead to symptoms or complications in every case. In some cases it can be completely symptom-free, so that it is diagnosed relatively late for this reason. For many of those affected, however, urogenital tuberculosis leads to very severe pain when urinating.
These pains are burning and have a very negative effect on the psychological state of the patient, so that sometimes depression or other psychological upsets can occur. Flank pain can also occur and make everyday life difficult for the person affected. The urine is bloody in urogenital tuberculosis, which can also lead to a panic attack.
The disease also leads to flatulence or constipation and greatly reduces the patient's quality of life.In women, the disease can also lead to heavy menstrual bleeding and pain. In most cases, urogenital tuberculosis can be treated relatively easily with the help of medication.
No particular complications are to be expected. Those affected, however, are dependent on prolonged use of the medication. If treatment is successful, the patient's life expectancy will not be negatively reduced.
When should you go to the doctor?
Since urogenital tuberculosis cannot heal itself, the person affected should consult a doctor at the first symptoms or signs of the disease. Only with early diagnosis and treatment can further complications or further worsening of the symptoms be avoided. A doctor should be contacted if the patient experiences painful urination. There is usually a slight burning sensation or itching.
In many cases, urogenital tuberculosis is also noticeable in bloody urine. Some people also suffer from constipation or flatulence and thus from a significantly reduced quality of life. In women, urogenital tuberculosis can also lead to intermenstrual bleeding or to a disturbed cycle. A doctor should also be contacted if the symptoms persist and do not go away on their own. As a rule, urogenital tuberculosis can be treated well by a urologist.
Treatment & Therapy
The standard handling of the Urogenital tuberculosis takes place today through combination therapy. Isoniazid, rifampicin and pyrazinamide are usually used. If necessary, these active ingredients can also be combined with ethambutol. The therapy must be continued consistently over a longer period of time. Normally six months can be assumed.
If the therapy is ineffective, surgical resection is usually required. This is especially true if urogenital tuberculosis has led to the development of a putty kidney or hydronephrosis.
You can find your medication here
➔ Medicines for bladder and urinary tract healthprevention
Since the Urogenital tuberculosis If it is a secondary disease, direct prevention is not possible. The most effective prophylaxis therefore consists in avoiding a primary infection or diagnosing it as early as possible.
Because the earlier a primary tuberculosis infection, for example in the lungs, is discovered and treated, the lower the risk that pathogens will settle and that organ tuberculosis such as urogenital tuberculosis will develop.
Aftercare
Follow-up care after a urogenital tuberculosis has been overcome depends on the therapy used. Since it is not a primary but a secondary disease, there is no risk of infection, which simplifies behavior during the drug treatment, which can last up to 18 months. Normally, the disease heals during long-term therapy.
It is crucial that the patient strictly adheres to the instructions for taking the medication, even if this is associated with unpleasant side effects. Follow-up care after successful medication is then mainly aimed at strengthening the body's immune system in order to avoid relapses as far as possible. Despite the actual or apparent healing of the urogenital tuberculosis, a further follow-up treatment consists of self-observation.
If symptoms appear that suggest a possible return of the disease, a wide variety of examination methods can clarify the situation. It then turns out whether it is a false alarm or whether one of the organs in question is affected. In some cases, even more advanced findings can then arise.
They indicate the need for immediate action. This may not only consist of a new medication phase, but surgical interventions may also be necessary to remove stenoses or to interrupt and stop the progression of urogenital tuberculosis in certain organs. These serious cases also require parallel treatment with medication.
You can do that yourself
Urogenital tuberculosis is treated with medication. The most important self-help measure is compliance with the medical guidelines for taking the medication. Typically used preparations such as isoniazid or rifampicin often cause side effects such as gastrointestinal disorders or allergies. If symptoms of this kind are noticed, a visit to a doctor is recommended.
After six months of combination therapy, the urogenital tuberculosis should have subsided. If the treatment does not work, a surgical attack is necessary. After the operation, the surgical wound must be carefully observed so that any inflammation or bleeding can be treated quickly. In the event of complications, a quick medical clarification also applies here. At the same time, the patient should cool the affected area well and care for it carefully. The doctor can prescribe suitable disinfectants with which the wound can be optimally treated. If necessary, natural remedies from the homeopathic field can also be used. This must first be discussed with the treating doctor.
Urogenital tuberculosis can significantly reduce well-being, which is why the focus after the illness is on regaining quality of life. Patients can now resume hobbies, lifestyle habits and professional activities that were neglected during the several months of therapy.








.jpg)

.jpg)
.jpg)











.jpg)