If there is persistent loss of visual acuity associated with tearing and redness in one or both eyes, an ophthalmologist should be consulted for an Uvetitis to exclude.This inflammation of the vascular skin can affect patients regardless of age and should be treated immediately to avoid permanent damage to the eye.
What is uveitis?
A Uveitis is a Inflammation of the vascular skin of the eye. The eyeball is a structure that is lined with three layers of tissue, with the layer in the middle denoting the vascular skin (uvea). The inflammation can affect certain areas of the uvea.
This results in a distinction between anterior, intermediate and posterior uvetitis, with anterior uvetitis being the most common form of inflammation of the vascular skin and also referred to as iritis or inflammation of the iris. The disease can be a one-off or chronic. There are no age limits for the affected patients.
The symptoms that occur include dull pain in the eye, which can radiate to the forehead. The eye is red and watery. Visual acuity is usually reduced and there is a sensitivity to light. With chronic uvetitis there are often fewer symptoms. The disease can occur in one eye or on both sides.
causes
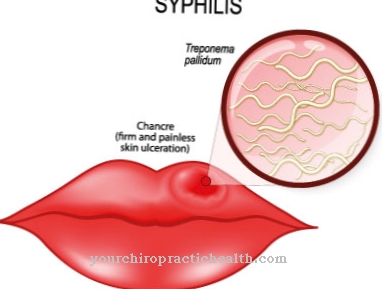
Cause for a Uvetitis can be bacteria as well as viruses, fungi and parasites. Viruses include herpes or varicella. The inflammation can also occur during tuberculosis or borreliosis.
It is often the result of another illness that has already been overcome, such as a bacterial diarrheal illness caused by Yersinia. Various autoimmune diseases also promote uvetitis. These include the chronic intestinal diseases Crohn's disease and ulcerative colitis as well as rheumatic diseases such as juvenile arthritis, ankylosing spondylitis and sarcoid, multiple sclerosis or certain kidney infections.
However, often no causes for the occurrence of the disease can be found. It is assumed that in these cases it is an immune reaction of the body to certain protein structures of the eye, which are regarded as foreign and thus trigger the uvetitis.
Symptoms, ailments & signs
Uveitis can be acute or chronic. In the chronic forms of the disease, however, acute relapses with symptom-free intervals are possible. The most important sign is a sudden or slowly developing deterioration in vision. Those affected see increasingly blurred. The visual acuity decreases.
In addition, there is often severe pain. Very rarely the iris can be colored differently. Depending on where the skin of the blood vessels is inflamed, there may also be significant reddening of the eye with strong tearing and increased sensitivity to light (dazzling). This is especially true if the front part of the [inflammation of the eye is inflamed]].
A basic distinction is made between three types of uveitis. So there is an anterior, middle and posterior uveitis. The posterior uveitis is usually only characterized by blurred and unclear vision. Pain, reddening of the eyes and tears do not usually occur here. Uveitis is usually very treatable.
However, in some cases it can become chronic. Then later recurrences occur more often. Sometimes adhesions of the iris with the lens or the chamber angle are also possible. Visual impairments due to vitreous opacity, cataracts or glaucoma also occur. If the retina or choroid are involved, the retina can be destroyed, which can lead to night blindness or even complete blindness.
Diagnosis & course
The diagnosis of Uvetitis says the ophthalmologist. By interviewing the patient, he already receives initial indications of a possible skin inflammation. The diagnosis can be confirmed by a thorough examination of the fundus. Blood tests may also be necessary to identify further infections that may be the cause of the skin inflammation.
A one-time uvetitis usually heals without any further consequences for the patient. However, if the infection recurs and chronic inflammation develops, damage to the eye can be expected, which will permanently reduce visual acuity.
Complications
Different complications can occur depending on the type of uveitis. A typical complication of anterior uveitis is inflammation in the anterior section of the vascular skin, which is associated with visual disturbances and occasionally with scarring and permanent impairment of vision. In addition, the iris and the lens can stick together. A so-called glaucoma occurs as a result of an increase in intraocular pressure.
With moderate uveitis, fluid can collect on the retina and sometimes tear the retina. Cataracts or glaucoma can also occur. When the posterior uveitis is inflamed, the retina is also often damaged - visual disturbances that can be chronic.
Other possible complications are clouding of the lens of the eye (cataract) and the accumulation of calcium in the cornea. In infants and young children, uveitis is often severe and causes permanent damage to the eye. Injuries to the eye can occur during an operation. Infections may also occur or the eye may not heal properly after the procedure and become infected again. Laser therapy carries similar risks.
When should you go to the doctor?
A doctor should be consulted if symptoms in the eye area persist or increase. Watery eyes, redness and irritation indicate inconsistencies that must be checked and treated. If there is impairment of vision, pain or an increased risk of accident, a doctor is required to clarify the cause. If the person concerned suffers from sensitivity to the effects of light, blurred vision or dizziness, a visit to a doctor is advisable. If night blindness is noticed or headaches occur regularly, research into the cause should be carried out.
Sudden changes in normal eyesight are considered worrying. You should be examined by a doctor as soon as possible. Disturbances in the tear duct, swelling around the eyes or itching should also be presented to a doctor. Since it can lead to complete blindness if left untreated, a doctor should be consulted as soon as the first irregularities occur. In addition, a check-up visit to a doctor is generally recommended if a difference in vision is perceived in everyday life in direct comparison with people from the social environment.
Unsteady gait, abnormal behavior or mood swings indicate health impairments that should be discussed with a doctor. Often, due to the functional disorders of the eye, psychological irregularities occur in parallel, as the emotional burden on the person concerned is very strong.
Treatment & Therapy
Treatment of the Uvetitis depends on the cause of the disease. The ophthalmologist selects medications to help reduce inflammation and prevent long-term damage to the eye. If the cause is bacterial, antibiotics are prescribed; A cortisone ointment is usually prescribed to reduce inflammation.
It is also important to avoid sticking to the iris. To do this, the pupil must be dilated with appropriate eye drops (cycloplegics or mydriatics). If the immune system is disturbed, the immune reaction is dampened with cortisone. Depending on the type of inflammation, the drugs are given as eye drops, in tablet form or as an injection.
Most patients cure the uvetitis with the administration of cortisone. If the inflammation does not recede sufficiently, other drugs are available that can intervene in the inflammatory process of the skin inflammation and thus achieve its healing. Only in particularly severe cases of uvetitis is an operation on the vitreous humor necessary.
You can find your medication here
➔ Medicines for eye infectionsprevention
There is no effective prevention against one Uvetitis, as this inflammatory reaction can have many causes. However, it is necessary to see an ophthalmologist immediately if there are discomforts to the eye that are accompanied by a decrease in visual acuity, so that uvetitis can be diagnosed and treated quickly. This is especially important for patients with chronic underlying diseases.
Aftercare
In order to avoid the development of secondary diseases, the treatment of uveitis should be followed by a comprehensive follow-up treatment. This consists of regular follow-up examinations at the ophthalmologist. This measures visual acuity, examines the fundus, as well as the skin, choroid, radiating body and iris and controls the intraocular pressure and takes countermeasures in good time in the event of a secondary disease or renewed uveitis.
If visual acuity is permanently impaired as a result of uveitis, glasses or contact lenses may be necessary. If the lens is cloudy as a result of uveitis, it must also be treated. If the intraocular pressure has increased as a result of uveitis or its treatment, it must be reduced with medication. For this purpose, special water tablets (Glaupax, Azemid) are used, which lower intraocular pressure.
If an infection with viruses, bacteria, fungi or parasites was the trigger for uveitis, increased personal hygiene should also be observed. In particular, you should refrain from rubbing your eyes with uncleaned or not disinfected hands. If there is an autoimmune disease that has resulted in uveitis, this must be treated separately in order to prevent the recurrence of uveitis and the development of secondary diseases of the eyes.
You can do that yourself
Home remedies are also suitable for relieving itching and redness in the affected eye. Cold or warm compresses are effective as an immediate measure. A clean cloth should be soaked in cold or lukewarm water. Then this compress should be carefully placed on the closed eye. The compress will help relax the affected eye.
The infection cannot be combated with it. Eye washes can help better. This is how pus can be washed out of the eye. One method of rinsing the eyes is to use a syringe without a needle that has been drawn up with lukewarm water. In doing so, the water should be dripped slowly into the eye with only slight pressure so that the cornea is not damaged.
Toppers with chamomile tea are also a proven means of improving symptoms in uveitis. To do this, water should be boiled and steeped with chamomile tea for five to ten minutes. However, it is important that it is not chamomile tea from the supermarket, but pure chamomile from the pharmacy or a health food store. A clean cloth should be soaked in the lukewarm or even cold chamomile brew for the topping. This moist pad should then be placed on the affected eye. This is how the chamomile compress can develop its healing and beneficial effects.


.jpg)
.jpg)






.jpg)

.jpg)
.jpg)











.jpg)