A Vein weakness, Venous insufficiency or that Vein problems is declared a widespread disease and can appear at a very young age. However, venous insufficiency does not necessarily have to be a typical age-related disease. In addition, vein problems can be prevented well.
What is vein weakness
A Venous weakness (vein problems) manifests itself through various signs of illness that have a more or less severe impairment of well-being and quality of life.
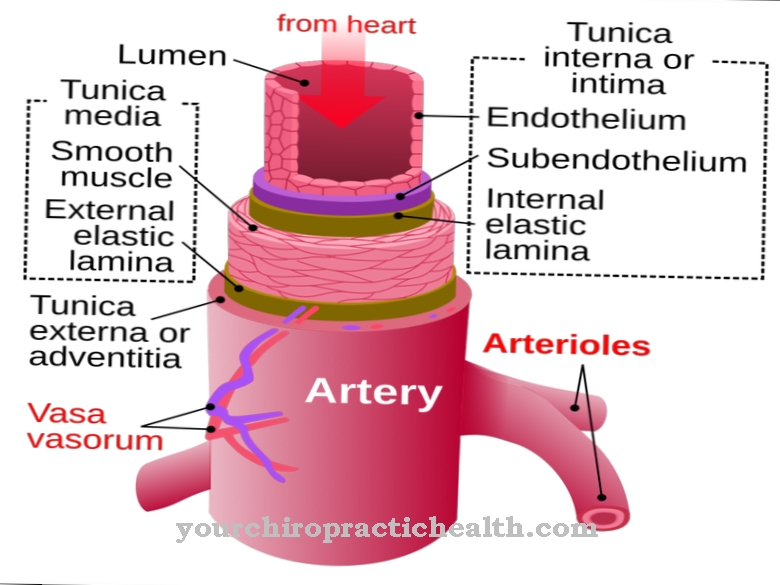
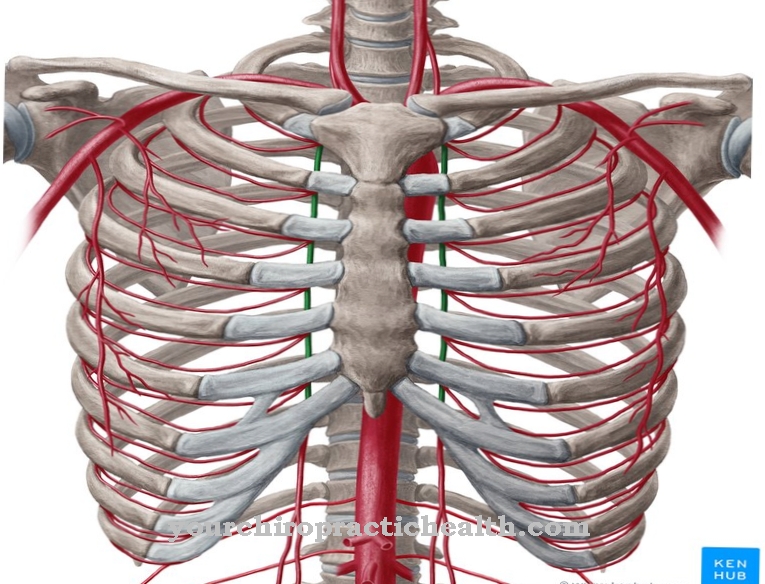
Based on the disease name Vein weakness it becomes clear that symptoms appear in the area of the blood vessels, the veins. The venous weakness is usually based on a limited ability of the veins to pump the oxygen-poor and high-slag blood from the legs back to the heart.
The blood "sinks" in the lower extremities and leads to the typical symptoms. If left untreated, the venous disease can develop into a serious and health-threatening disease. The functional restriction of the veins thus leads to extensive consequential damage if no suitable therapy is given.
causes
The causes of a Vein weakness are clearly known these days. The so-called risk factors, which are to be looked for in external and internal circumstances, are important for venous disorders.
In order to constantly strengthen the veins, it is essential to move physically. A lack of exercise and the associated obesity can lead to weak veins. Constant sitting or standing at work and in leisure time means that the legs are seldom challenged by walking. This can then easily lead to weak veins.
For women, pregnancy and various medications such as birth control pills are considered increased risk factors. A special situation that can contribute to a venous weakness without appropriate prevention is a surgical procedure with an associated long hospital stay.
Hereditary predisposition and an increased willingness of the blood to clot are also among the causes of weak veins.
Symptoms, ailments & signs
The weak veins are generally expressed by tired and heavy legs. In the early stages, however, no symptoms appear. Without treatment, however, the disease progresses and can eventually lead to open legs. Venous disease is usually accompanied by feelings of tension and heaviness in the legs.
At the same time, there is swelling because water accumulates in the legs. Pain occurs after standing or walking for a long time.Often there are also foot and calf cramps. Patients also often experience itching of the legs. In severe cases, eczema and lower leg ulcers develop.
Since the disease progresses in stages, with the exception of the most severe stage, not all symptoms are usually observed at the same time. The venous weakness is divided into seven stages. At the beginning, in stage C0, there are still no symptoms. So-called spider veins then appear in the subsequent stage C1. These are the finest spider-web-like vein drawings that look reddish to bluish.
In the following stage, varices (varicose veins) appear on the lower legs, calves or hollows of the knees. Stage C3 is then characterized by swollen legs due to water retention. As the disease progresses, skin changes occur. Brownish skin pigmentation appears, especially in the area of the ankles. The skin is flaky and itchy. Ultimately, open sores develop that are difficult to heal. The risk of developing a thrombosis increases sharply.
Diagnosis & course
A Vein weakness is, besides the smoker's legs, popularly known as intermittent claudication because the painful complaints force those affected to linger constantly.
Not every venous disease is life-threatening, but is characterized by a rather harmless course. Nevertheless, a weak vein must be treated in any case. The gradually appearing heavy and tired legs, abnormal sensations in the legs, varicose veins and later blood clots include dead skin areas, a thrombosis and a life-threatening pulmonary embolism.
In addition, the water retention in the legs, deep ulcers and swollen ankles are significant signs of venous weakness for the diagnosis.
Complications
A weak vein can cause discomfort in different parts of the body. First and foremost, there is severe pain in the legs. The legs feel heavy and those affected can no longer actively participate in everyday life. Swelling in the legs can also occur due to the weak veins and have a very negative effect on the patient's quality of life.
Many of those affected continue to suffer from cramps in their calves or from severe itching on their legs. These symptoms occur frequently, especially at night, and can lead to sleep problems and irritation in the patient. The legs can also tingle or feel numb. In severe cases, weak veins also lead to paralysis or impaired sensitivity.
If the complaints are not treated, water may also be retained in the legs. The treatment of weak veins can take place with the help of medication and compression stockings. There are no complications. However, those affected are dependent on lifelong treatment. Life expectancy remains unaffected by the disease.
When should you go to the doctor?
If the veins become more and more blue, countless spider veins have formed, or if the legs feel heavy and swollen, you should definitely see a doctor. This can be the family doctor, who may refer you to a specialist, or the phlebologist, the specialist in venous diseases, can be contacted immediately. Even if the veins are already inflamed and the leg hurts, it is urgent time to see a doctor.
In addition, it makes sense not to postpone the doctor's visit that far in the first place. Anyone who knows that they have weak connective tissue and weak veins should consult a doctor in good time. After examining the state of the disease, he or she specifies the frequency of the check-ups, for example every two years, and will recommend suitable preventive measures. Compression stockings are usually prescribed. This gives you another reason to see a doctor: If these tight-fitting stockings are broken and / or new ones are needed, a visit to the doctor is also essential.
Treatment & Therapy
Depending on the first noticeable symptoms, timely therapy is already required Vein weakness actionable. This usually begins when the patients complain about complaints.
By raising the legs to relieve the leg veins and the heart as well as by wearing compression stockings and applying venous bandages every day, the course of the disease can be delayed and the symptoms relieved. Warm baths and regular exercise are also useful. Rubbing the legs with herbal medicinal products that promote increased blood flow leads to better well-being for many of those affected. Any varicose veins that occur can and even sometimes have to be removed surgically.
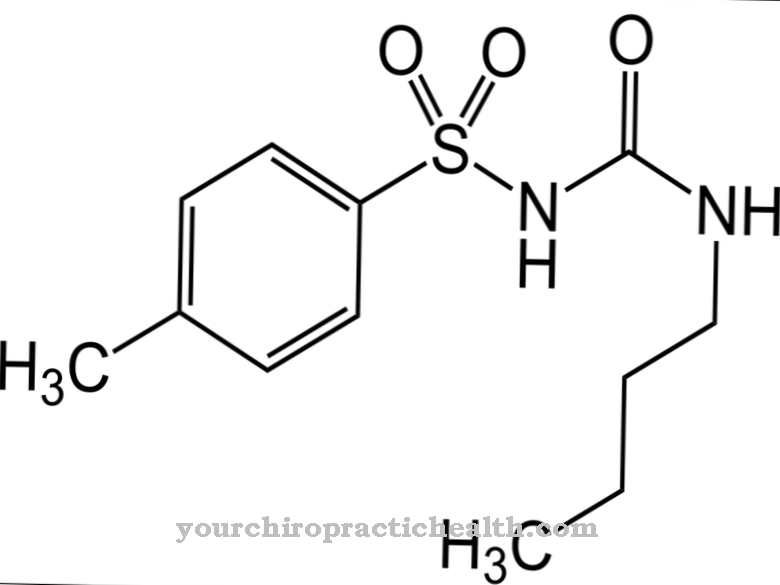
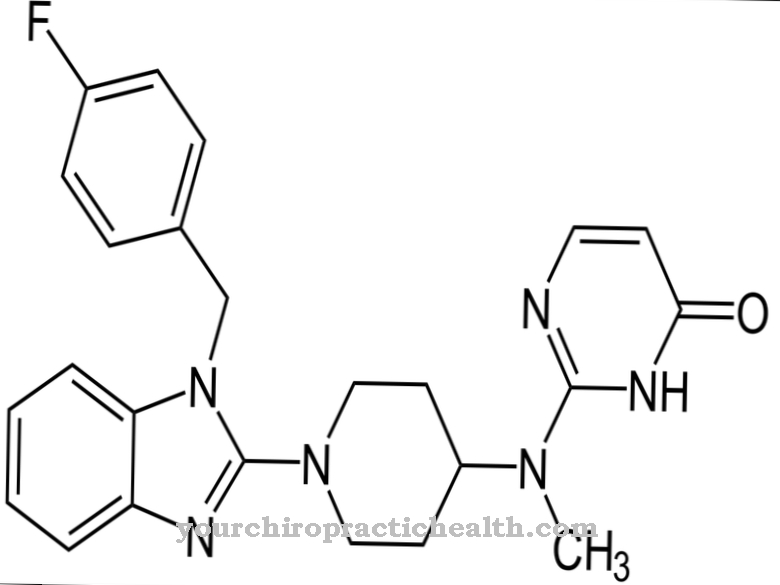
Supportive medical treatment for weak veins includes administering medication to increase the velocity of the veins. In order to prevent a thrombosis caused by the formation of blood clots, it is advisable to administer drugs from different active groups if the veins are weak.
These are supposed to reduce the fluid permeability of the leg veins in the form of so-called edema protectors. In venous disorders, diuretics help reduce water retention in the legs. As part of further therapeutic options, superficial veins can be surgically obliterated.
prevention
Not all patients can develop the Vein weakness be prevented. As a prophylaxis against venous disorders, sufficient physical exercise (sport), a healthy and balanced diet as well as the consideration of side effects and contraindications with drugs are central aspects. Measures to stimulate blood circulation in the context of physiotherapeutic methods and wellness are also beneficial to counteract weak veins.
Aftercare
If the venous weakness has to be treated by surgery, appropriate follow-up treatment is important. The behavior of the patient after the operation also plays an important role. On the one hand, it makes sense for the patient to take it easy after the operation, but on the other hand, he should move slightly.
Medical check-ups are required after the vein operation. There is a risk of after-effects such as swelling or inflammation of the veins. In some cases there is even a risk of blood clots and dangerous embolisms. As part of the follow-up examination, the doctor can identify such complications at an early stage and treat them accordingly.
The wearing of special compression stockings is an important part of aftercare. If the vein operation is optimal, the patient wears the stockings continuously for about a week. The special stockings support the healing process and are therefore considered indispensable.
After the first week, the patient only needs to wear the compression stockings during the day for the next five weeks. Sometimes it may be necessary to apply a compression bandage after the procedure, depending on the extent of the operation. Light movement is also an advantage. However, the patient must pay attention to the correct amount and take regular rest breaks in order to protect the veins. Light walks and everyday household movements are considered sensible.
You can do that yourself
Which treatment the doctor suggests for a weak vein depends on the symptoms. Usually, the patient has to wear compression stockings, which put pressure on the veins in the legs and relieve the venous valves. In addition, special compression stockings prevent fluid from sinking into the tissue, which in turn reduces swelling. Special pressure dressings are equally effective.
Sufficient exercise is recommended as a support, whereby gentle sports such as aqua jogging, swimming or walking on soft surfaces are recommended. At least 30 to 45 minutes of exercise per day are necessary to effectively counteract venous weakness. Sitting for long periods, especially with knees bent, should be avoided. Alternatively, the legs can be relieved through special ball training.
In standing professions, there are exercises such as wiggling your toes or circling your feet. The load on the feet should be reduced again and again, for example by placing one foot on a pedestal. Pronounced weak veins are usually treated with medication. The most important self-help measure here is to monitor the side effects and interactions of the prescribed medication.

.jpg)






.jpg)
.jpg)
.jpg)







.jpg)