ammonia is the chemical compound of hydrogen and nitrogen. The molecular formula of ammonia is NH3. The substance is created in the body when proteins are broken down.
What is ammonia?
Ammonia is a colorless gas made up of three hydrogen atoms and one nitrogen atom. The gas has an extremely pungent odor. Ammonia is toxic to the human body. It is usually present there as a water-soluble salt.
In this form it is also called ammonium (NH4 +). Ammonia is involved in various metabolic processes. However, it occurs particularly when protein is broken down in the intestine. Ammonia is also produced during cell metabolism and the breakdown of amino acids. Ammonia can seriously damage the cells of the body. It is therefore converted to urea in the liver and then excreted in the urine via the kidneys.
Function, effect & tasks
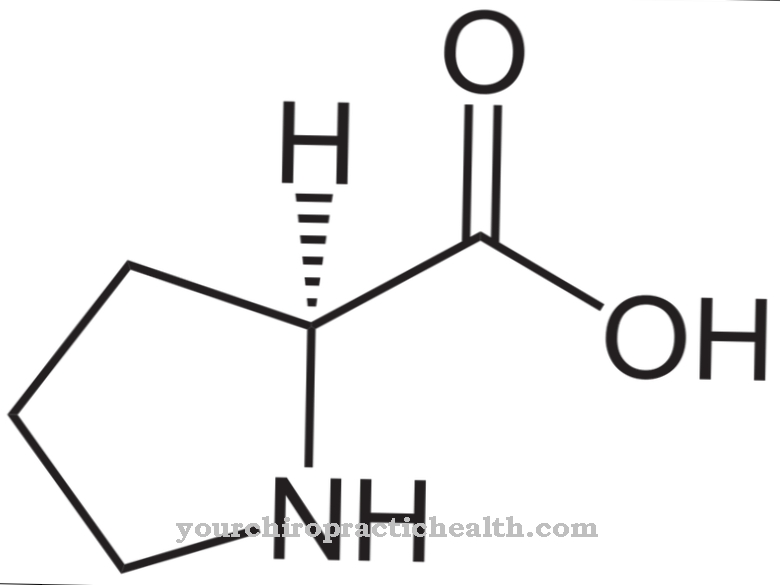
Ammonia plays an important role in the metabolism in building and breaking down amino acids. However, in these metabolic processes, the ammonia is in the form of ammonium.
Ammonium and α-ketoglutarate are converted into glutamate in a special chemical process known as reductive amination. Glutamate, also known as glutamic acid, is an α-amino acid. Since the body can produce glutamic acid itself with the help of ammonium, it is one of the non-essential amino acids. As an amino acid, glutamic acid is also an important component of proteins. Through the process of transamination, other non-essential amino acids can be produced from glutamate.
Glutamate is not only involved in amino acid synthesis, it is also one of the most important excitatory neurotransmitters in the central nervous system (CNS). At the same time, the amino acid is also the precursor of γ-aminobutyric acid (GABA). This in turn is the most important inhibitory neurotransmitter in the central nervous system. Glutamate is also said to have a positive effect on muscle growth and the immune system.
Education, occurrence, properties & optimal values
A large part of ammonia is produced when amino acids are broken down. The main place of production of free ammonia is the intestine. In the large intestine in particular, ammonia is produced from undigested protein through the action of bacteria. The amino acids are first broken down again into glutamate.
This amino acid is then split into the original substances α-ketoglutarate and ammonia by the enzyme glutamate hydrogenase. Not all of the ammonia that is created in this way can be used to rebuild amino acids. In larger quantities, ammonia also has a cytotoxic effect, so that the body must be able to break down ammonia. Organisms that are native to the water can often release ammonia directly through their skin into the surrounding water. Before excretion, humans must convert the toxic ammonia into a non-toxic form. With a healthy liver, ammonia is absorbed quickly.
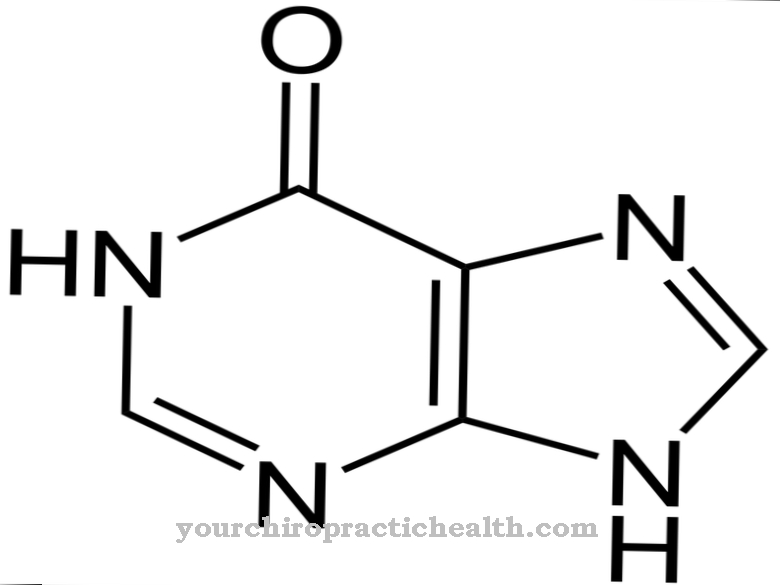
This usually reaches the liver via the portal vein. The liver then converts ammonia or ammonium into urea (urea). Urea is a white, crystalline and non-toxic substance. It is excreted in the urine via the kidneys.
The normal plasma value for ammonia is 27 to 90 μg ammonia / dl. This corresponds to an amount of 16 to 53 μmol / l. The ammonia levels in the blood are usually determined as part of an examination of the liver function.
Diseases & Disorders
Decreased ammonia levels in the blood serum are of no clinical relevance. Increased ammonia levels usually occur with decreased liver function. The breakdown of ammonia is greatly impaired in cirrhosis of the liver.
Liver cirrhosis is the end stage of many liver diseases. The stage is irreversible and therefore cirrhosis of the liver cannot be cured. Usually cirrhosis develops over years to decades. In Europe, the most common cause of cirrhosis of the liver is alcohol abuse. Chronic viral hepatitis can also end in cirrhosis of the liver.
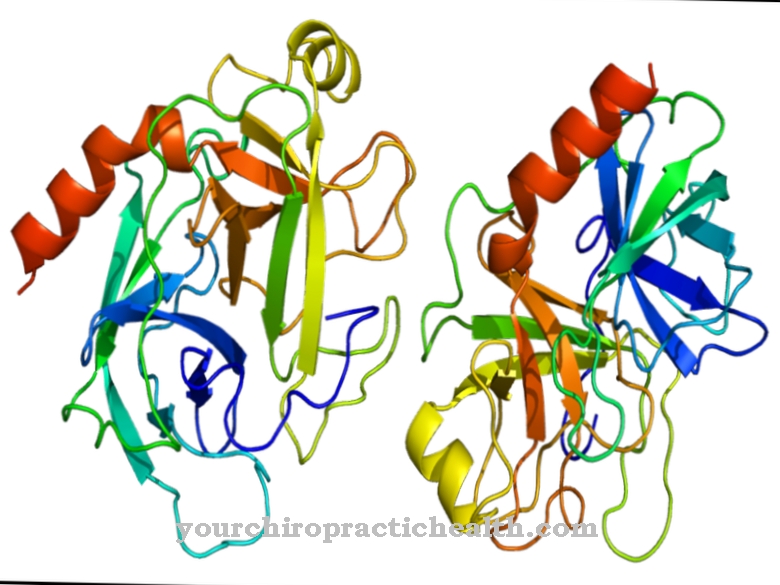
In cirrhosis, liver tissue is destroyed and the liver function cells are remodeled by connective tissue. On the one hand, this disrupts the blood flow to the liver. On the other hand, the liver cells can no longer fulfill their detoxification task. If the ammonia level increases significantly due to impaired liver function, hepatic encephalopathy can occur. This is a brain dysfunction due to the liver's inadequate detoxification function. The reason for this damage is probably the similarity of ammonium and potassium. When potassium and ammonium are exchanged, the so-called NMDA receptor is disrupted.
This in turn allows more calcium to penetrate the nerve cell. Cell death occurs. The hepatic encephalopathy can be divided into four stages. The four stages are preceded by latent or minimal hepatic encephalopathy. This manifests itself in poor concentration, reduced drive or memory difficulties. In the first stage there is a noticeable reduction in the level of consciousness, a clear drive disorder and a disorder of fine motor skills. In the second stage, those affected suffer from disorientation, memory disorders, slurred speech and severe sleepiness.
The third stage is associated with severe impairment of consciousness, loss of orientation, muscle stiffness, stool and urinary incontinence and unsteady gait. The most severe form of hepatic encephalopathy is hepatic coma (stage 4). The patients are unconscious and can no longer be awakened by pain stimuli. The muscle reflexes are completely extinguished.
Because of the penetrating smell, poisoning by gaseous ammonia is rather rare. Ammonia in gaseous form is mainly absorbed through the lungs. By reacting with moisture, it has a strongly corrosive effect on the mucous membranes of the respiratory tract. Above a certain concentration there is a danger to life. The ammonia can lead to laryngeal edema, glottis spasms, pulmonary edema or pneumonia and thus cause respiratory failure.







.jpg)

.jpg)
.jpg)











.jpg)