Antidiabetic drugs are required when the body is unable to regulate blood sugar levels using its own insulin.
What are antidiabetic drugs?

Antidiabetic drugs are medicines used to treat the metabolic disease diabetes mellitus (diabetes). In a healthy body, the "beta cells" in the pancreas produce sufficient insulin. Insulin ensures that the body absorbs sugar and thus reduces the blood sugar level as soon as it rises after the ingestion of carbohydrate-containing food.
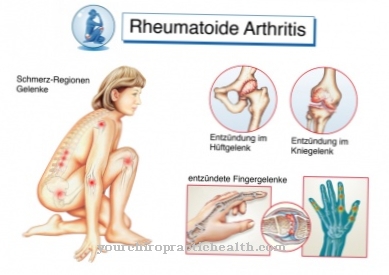
Type 1 diabetes is an autoimmune disease in which the immune system mistakenly attacks and destroys the "beta cells" in the pancreas, causing a decrease in insulin production. Type 2 diabetes, on the other hand, is characterized by “insulin resistance”: Insulin that may be present in the body does not work properly at its target locations, so that the blood sugar level cannot be broken down sufficiently.
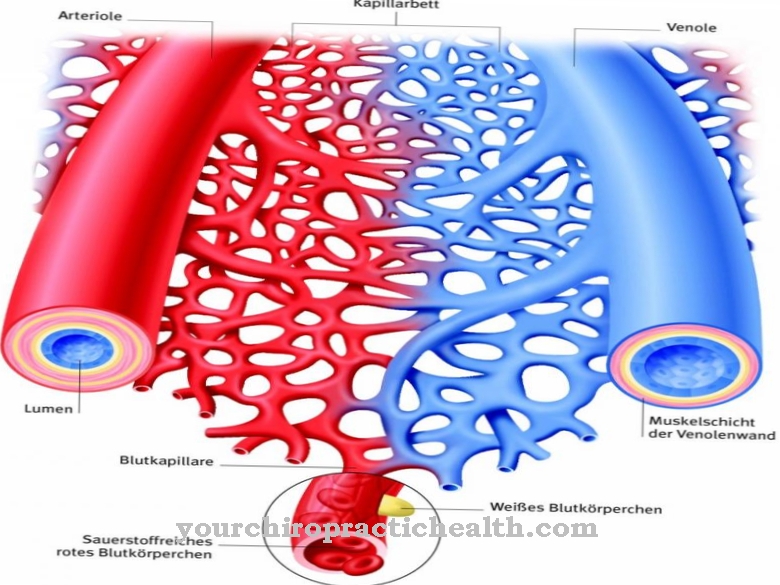
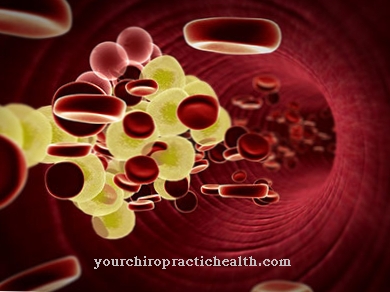
In type 2 diabetes, both sufficient and limited insulin production is possible. If no antidiabetic drugs are taken in diabetes mellitus, a permanently high blood sugar level leads to damage to blood vessels and nerves and to circulatory disorders.
Blindness, stroke and heart attack can occur as secondary diseases. Serious circulatory disorders due to diabetes sometimes require amputations if the treatment with antidiabetic drugs is not timely.
Medical application, effect & use
Antidiabetic drugs are only used if other forms of therapy, such as a change in diet or increased physical activity, do not lower blood sugar levels sufficiently.
According to their mode of action, antidiabetic drugs are classified as either "insulinotropic" (promoting insulin secretion) or non-insulinotropic drugs: either antidiabetics improve the breakdown of sugar after eating or they cause an immediate supply of insulin. Insulinotropic antidiabetic drugs are primarily used in type 1 diabetes to compensate for or stimulate the body's own insulin production which is too low, as far as this is possible due to the availability of sufficient beta cells.
Non-insulinotropic anti-diabetic drugs are used in type 2 diabetes when the body makes enough insulin, but the insulin does not work. If the body produces too little insulin in the presence of insulin resistance (type 2 diabetes), treatment is also carried out with an insulinotropic antibiotic.
Depending on their form of administration, a distinction is made between oral (ingested through the mouth) and parenteral (mostly administered by injection under the skin or by infusion into the bloodstream) and antibiotics taken in through inhalation. Oral antidiabetic agents are primarily used for type 1 diabetes, non-oral antidiabetic agents for type 2 diabetes.
Herbal, natural & pharmaceutical anti-diabetic drugs
To the oral Antidiabetic drugs belong u. a. the "alpha-glucosidase inhibitors". Glucosidase is an enzyme that breaks down complex sugar and starch molecules during the digestion of food in the small intestine and thus ensures that sugar is quickly distributed in the blood. (Enzymes are proteins that accelerate certain biochemical processes.)
Glucosidase inhibitors prevent a rapid increase in blood sugar after meals. “Biguanide” drugs, on the other hand, reduce sugar production in the liver and also inhibit the release of sugar. "Glitazones" cause an increased formation of proteins, which ensure that sugar is transported from the bloodstream into the cells. "Glinide" have a short duration of action and are therefore taken about thirty minutes before a meal in order to stimulate the production of insulin precisely during a digestive process.
Sulphonylureas block potassium channels in the beta cells of the pancreas and thus enable an increased release of insulin. The main non-orally administered anti-diabetic drugs include insulin, which is injected under the skin or into a vein. Hundreds of medicinal plants also have an antidiabetic effect, some of which has been proven in clinical studies. The plant parts that act like antidiabetic agents include the shells of the kidney beans, the leaves of the blueberry and the fruits or seeds of the "Java plum".
Risks & side effects
The Antidiabetic drugs Alpha-glucosidase inhibitors can cause bloating, abdominal pain, gas, nausea, and diarrhea. Alpha-glucosidase inhibitors must not be used in chronic digestive disorders.
Possible side effects of biguanides include vomiting, nausea, diarrhea, and lactic acid poisoning. When taking glitazones, headaches, disorders of water excretion and accumulation of water in body tissue (edema formation) and mild anemia (anemia) can occur. Glitazone must not be taken at the same time as insulin is administered. Glinides sometimes trigger hypoglycemia (low blood sugar levels), which can lead to cravings, decreased brain performance, aggressiveness, seizures or shock.
Sulphonylureas present an even greater risk of hypoglycaemia. In addition, sulphonylureas are not compatible with alcohol consumption, in which, due to an accumulation of toxic acetaldehyde (an alcohol breakdown substance) in the liver, in addition to nausea, vomiting, headache, dizziness and itching, sweating, an increased heart rate (tachycardia) and low blood pressure (hypotension) may occur.
The consumption of sulfonylureas leads to an average increase in body weight of 2 kilograms. In some cases the number of red or white blood cells decreases (anemia or leukopenia) or the number of platelets decreases (thrombocytopenia).
Cross-allergies with sulfonamide antibiotics or with (diuretic) thiazides are also possible. Sulphonylureas must not be taken during pregnancy and in case of renal insufficiency. The effects of sulfonylureas are increased when insulin and beta blockers are administered at the same time, while the effects of these antidiabetic drugs are reduced when certain other drugs are taken at the same time.














.jpg)



.jpg)

.jpg)