A Conjunctivitis or Conjunctivitis is an inflammation of the conjunctiva in the eye. Especially the reddened eyes are a typical sign of conjunctivitis. The causes are varied and range from bacterial inflammation to allergic reactions. Viruses can also lead to conjunctivitis of the eye through infection.
What is conjunctivitis?

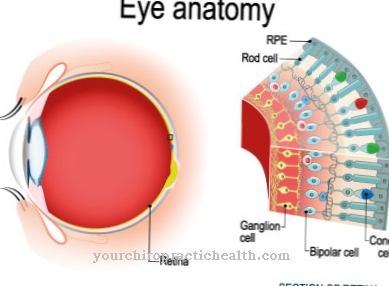
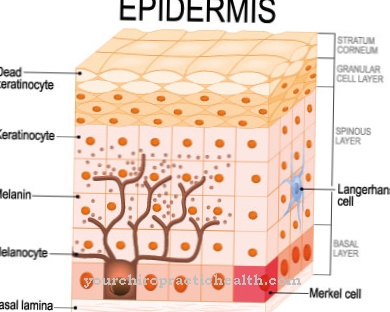
Conjunctivitis, or conjunctivitis, is inflammation of the conjunctiva of the eye. The conjunctiva itself covers the outer shell of the eyeball as well as the inner side of the eyelids. This transparent mucous membrane produces the moist, liquid mucus necessary for the eye, which adheres to the eye as a tear film. The point is less friction when moving and closing your eyes.
The conjunctiva is a thin, delicate and transparent mucous membrane that covers the inside of the upper and lower eyelids as well as the front half of the eyeball and ends at the edge of the cornea in the middle between the eyelids. While it is firmly attached to the underlying tissue on the inside of the eyelids, it lies loosely on the eyeball.
When the inside of the eyelids are folded over to the eyeball, the conjunctiva forms sack-shaped cavities, also called conjunctival sacs. Eye drops and eye ointments can be conveniently placed in the lower conjunctival sac for treatment if the lower eyelid is pulled downwards with the fingers and then turned outwards.
In the case of inflammation, the conjunctiva, which is transparent in the non-inflammatory state and makes the eyeball appear white with the exception of the cornea, is supplied with much more blood. It then takes on a red color and becomes opaque, so that the white leather skin underneath can no longer shine through and the eyeball appears reddened.
The conjunctiva is also responsible for the immune defense of the eye, so that in the case of conjunctivitis the cornea and eyelids can also become inflamed. Since the eyes or the conjunctiva are relatively unprotected in the body, they are often susceptible to external germs and stimuli.
From this point of view, it is hardly surprising that conjunctivitis is one of the most common diseases of the eye. The pronounced red eyes in conjunctivitis are particularly typical.
causes
Conjunctivitis can have many causes. Usually conjunctivitis is triggered by viruses, fungi, parasites (e.g. worms) or bacteria and is thus an infectious disease. Furthermore, allergies and environmental stimuli can also trigger conjunctivitis. These are mainly drafts, injuries, smoke, dust and substances.
In rare cases, conjunctivitis occurs as part of another eye disease. Age-related eye disorders are also a cause. Conjunctivitis can vary regionally and temporally with allergic causes, depending on the occurrence of allergens or pathogens.
As already mentioned, both external damage and internal diseases can be considered as causes. External damage includes, for example, harmful effects from dust, smoke, foreign bodies, chemical vapors, glare, poor or inadequate lighting conditions, drafts, irritation due to excessive rubbing of the eyes, etc. Heavy smokers and people who are forced to be around so-called Stopping chain smokers can also develop conjunctivitis.
Since conjunctivitis quite often tends to become chronic, it is necessary to get rid of the external harmful influences. Most external damage often leads to conjunctivitis, especially if the conjunctiva is already susceptible to a certain degree.
Such a susceptibility can be caused, for example, by a slight refractive error in the eyes, which the patient is not aware of because it causes only a slight visual impairment. If the right glasses or contact lenses are prescribed in these cases, the disease can be remedied very quickly. The same applies to people with normal vision after the age of 45, in whom so-called presbyopia begins.
Many of them fail to wear glasses when working close-up, or they use glasses whose lenses have already become too weak and thus subconsciously contribute to chronic conjunctivitis. When reading and writing you have to make sure that the field of vision is well lit, which can best be achieved with an adjustable floor lamp. However, the light must not dazzle.
In many cases, conjunctivitis is also caused by pathogens (bacteria). If the bacteria are very malignant, such as poisonous pus, diphtheria bacilli, gonorrhea, etc., a violent inflammatory process can pass from the conjunctiva to the cornea, melt it down, so to speak, and penetrate the inside of the eyeball. Only through intensive specialist treatment can such violent inflammatory processes be stopped and the eyes saved.
In the case of newborn children of sexually ill mothers, preventive measures prevent them from developing such an inflammation, which in earlier decades usually led to blindness. However, it is not uncommon for general infectious diseases such as measles, typhus, etc., to be accompanied by conjunctivitis. In all these cases, the pathogens must be determined with the help of microscopic examinations of the conjunctival secretion in order to be able to carry out a targeted treatment.
Finally, conjunctivitis can also be caused by numerous substances and agents that the patient comes into contact with and to which they are hypersensitive or allergic. These primarily include flour dust and other types of dust, e.g. also pollen and bee pollen, which can cause hay fever and conjunctivitis, cosmetics, oil fumes, gasoline, chemicals, etc., the latter of which very often get on the conjunctiva by rubbing eyes while working.
Hypersensitivity and allergies to certain foods, such as strawberries, tomatoes, etc., can also cause conjunctivitis. A severe runny nose is also often associated with this disease. In addition, the tear ducts can be blocked, which can also lead to persistent and annoying tearing and conjunctivitis.
Symptoms, ailments & signs
Conjunctivitis manifests itself through various symptoms. The first sign is the redness of the eye. Due to the increased blood flow to the conjunctival vessels, there is a visible, usually light red discoloration on the edge of the iris. If deeper layers are inflamed, the edge of the iris appears bluish to reddish.
In addition to the reddening, the tear duct secretes purulent or slimy secretion, which often makes the eye sticky. If the cause is an allergic reaction, the conjunctiva can swell. These so-called papillae are accompanied by a strong feeling of foreign bodies.
In the case of severe inflammation, spasmodic eyelid closure can also occur. Allergic conjunctivitis manifests itself as itching, sudden tears and accompanying symptoms such as runny nose and sneezing. With bacterial conjunctivitis, purulent accumulations can also occur in the corner of the eye. The viral form usually occurs on both sides and manifests itself in puffy eyes and severe itching.
Depending on the degree of inflammation, the eye tears to a greater or lesser extent and excretes mucus and purulent secretion mainly at night, which often causes the eyelids to stick together so that they can only be opened with great difficulty in the morning.
In severe cases, the eye can no longer be closed - the conjunctiva appears swollen and glassy. Viral or bacterial conjunctivitis can cause small bulges inside the eyelids. In addition, there is a sensitivity to light and an annoying burning sensation, itching and a certain foreign body sensation, as if there were sand in the eyes.
All of these appearances are at acute conjunctivitis particularly pronounced. At a chronic conjunctivitis however, they are only slightly developed. Sometimes reddening of the conjunctiva can only be seen on the inside of the eyelids, while the conjunctiva looks completely normal.
Correspondingly, the symptoms of chronic conjunctivitis are less pronounced and generally only occur in activities that strain the eye, for example reading, writing and watching TV plus a computer, as well as smoking or in rooms where people smoke colder weather, wind and bright sunlight.
course
Untreated conjunctivitis is usually mild. Due to the body's self-healing process, there are seldom serious consequences for the eyes and lifelong impairment of vision. Loss of visual acuity can only sometimes occur when the cornea of the eye has been injured or inflamed.
However, if pain occurs or further complications arise, a doctor should be consulted immediately.
Complications
Complications are more common with viral conjunctivitis than bacterial because it takes more time to heal and symptoms are more severe. Corneal opacity is a possible long-term consequence of conjunctivitis caused by viruses. This visual disturbance can vary in severity and, with greatly reduced transparency, have a considerably restrictive effect on eyesight.
The formation of scars near the lacrimal glands and ducts, particularly noticeable in the case of infection with chlamydia, also impairs the moisturizing of the eye. Chlamydia infections are also often chronic and make it necessary to treat the person's partner as well. Even with a bacterial inflammation, depending on the state of the immune system and the type of pathogen, consequences can occur that threaten to blindness.
The cornea can become inflamed, as can the bags under the eyes. They are located in the inner corner of the eyelid. Secondary diseases such as otitis media or meningitis are also possible. In any case, it is advisable to carry out treatment with eye drops or antibiotics, imposed by the doctor, until the end of the prescribed days. Even if the symptoms improve, premature termination can lead to renewed inflammation of the conjunctiva.
When should you go to the doctor?
If the eyes are reddened, burned or itchy in certain situations, for example after long work at a computer screen or when staying in a strongly heated room, this is not yet a cause for concern. A doctor does not have to be consulted under these conditions. As a rule, a walk in the fresh air is enough for the eyes to recover. However, there are a number of situations in which burning or red eyes should be presented to the doctor immediately.
Conjunctivitis caused by pathogens such as bacteria, viruses or fungi are usually highly contagious. If your child comes home from daycare or school with reddened or irritated eyes, it is very likely that they have conjunctivitis. In this case, a doctor's visit is strongly recommended. If the suspicion is confirmed, the school management should be informed.
The doctor must always be consulted if changes in the eye occur after a trip abroad to tropical regions. In this case, the person concerned could have become infected with a dangerous parasite. Herpes infections that spread to the eye can be particularly unpleasant and dangerous. In these cases, a doctor must be consulted immediately to prevent serious complications, including loss of vision.
Doctors & therapists in your area
Treatment & Therapy
The treatment or therapy of conjunctivitis depends on its specific cause. In addition, the severity and course of the disease are also important in the treatment. A distinction is therefore made between the treatment on the basis of bacterial and viral causes as well as external stimuli and allergic conjunctivitis.
Depending on the numerous causes, there is a whole series of treatment instructions. In general, the general practitioner or ophthalmologist will initially prescribe mild disinfecting and anti-inflammatory eye drops and eye ointments, because they will cure the majority of patients. However, in many cases it is necessary to try several or a series of remedies.
Since it is only possible to determine more serious causes through repeated ophthalmological examinations, especially those suffering from chronic conjunctivitis should be advised to visit the ophthalmologist again and again even if the previously prescribed medication has not helped. In addition, however, everyone affected should endeavor to eliminate the damaging influences, be it at work or at home.
In the case of conjunctivitis caused by bacteria, no further treatment is usually necessary because it heals on its own. Nevertheless, the doctor may prescribe antibiotic eye drops or ointments that have a supportive effect. Antibiotics should only be used in severe cases. These can then be given as tablets or eye drops.
There is no direct treatment for conjunctivitis caused by a virus. Only manually administered tear fluid and cold compresses can alleviate the symptoms. The same procedure applies to conjunctivitis caused by external stimuli such as a draft.
If there is an allergic cause, substances that trigger allergies, such as pollen, should be avoided. Here, too, cold compresses and artificial tears help against the acute symptoms. For a lasting improvement, the doctor prescribes antihistamines or mast cell stabilizers. As with all forms of allergy, a desensitization against the causative allergens is a good idea.
Outlook & forecast
The course and prognosis of conjunctivitis can vary greatly depending on the cause of the disorder and personal circumstances.
Simple bacterial inflammation of the conjunctiva is almost always successfully treated with eye drops containing antibiotics after the pathogen has been identified. The symptoms usually resolve completely within a few days. However, the prerequisite for this is that the patient strictly follows the treatment instructions of his doctor.
In particular, the eye drops should not be taken off without authorization once the symptoms have disappeared. The treatment usually has to be carried out over a longer period of time in order to completely cure the inflammation and to avoid relapse. A new outbreak of the infection often leads to a more severe course, and conjunctivitis can also become chronic.
Conjunctivitis caused by viruses is more difficult to treat, and recovery can often take weeks. During this time, symptoms such as reddened, watery or painful eyes can occur again and again. However, viral infections usually heal without any long-term effects.
In exceptional cases, especially in people with a severely compromised immune system, the course can be very severe and persistent, although blindness due to conjunctivitis cannot be completely ruled out. However, this complication now occurs almost exclusively in patients in the developing world.
Aftercare
Conjunctivitis is a disease that can flare up again and again after it has subsided. Consistent follow-up care is recommended in advance to protect the eyes and avoid discomfort. This can be done by the patient himself or by an ophthalmologist. Even the experienced family doctor can examine the eyes for the condition of the conjunctiva in uncomplicated cases. If necessary, he advises to visit the family doctor again.
Follow-up care primarily involves protecting the sensitive conjunctiva of the eye from further irritation. When washing your face, you should avoid using harsh detergents, especially those with a high alcohol content. In addition, it is best to refrain from putting on make-up for a while to avoid particles of kohl, mascara or eye shadow from getting into the eyes.
Anyone who sweats a lot while exercising can use a headband to prevent drops of sweat from flowing into their eyes. Pollen allergy sufferers who have developed conjunctivitis through contact with pollen should avoid the allergens as much as possible during follow-up care. If the conjunctivitis is caused by exposure to sunlight, for example in high mountains, sunglasses are a valuable companion in aftercare. Medicines that the ophthalmologist has prescribed for local use can also be used in the follow-up after consultation. The same applies to means for eye moisturizing.
You can do that yourself
Medical treatment of conjunctivitis can be supported by various home remedies and self-help tips. One of the most important measures is increased hygiene. On the one hand, this prevents the inflammation from spreading to the other eye and to other people. On the other hand, lukewarm water reduces the pressing feeling of foreign bodies and quickly flushes out pathogens. Alternatively, an eye bath, in which the eye is dipped in a glass of water, can also help.
In the case of severe inflammation, it is recommended to wear protective goggles. In general, contact with stimuli such as wind, chlorinated water, smoke or extreme cold or heat should be avoided. Antiseptic agents (such as bibrocathol, povidone and zinc sulfate) from the pharmacy have anti-inflammatory effects and help especially in the first few days of inflammation.
In the further course, painful eye rims can also be dabbed off with a little black tea. Other proven home remedies are, for example, eyebright, rue, marigold ointment or quark compresses. Tip: use woolen towels or disposable handkerchiefs to dry your eyes, which are disposed of after use.
If the inflammation spreads anyway or has not subsided after a week at the latest, another visit to the ophthalmologist is recommended.






.jpg)