The Ulcerative colitis is a chronic inflammation of the bowel that can occur in flares. It usually begins in the rectum and then spreads to the entire colon. Typical signs are purulent and slimy diarrhea, which is sometimes accompanied by blood. There is also severe abdominal pain and weight loss. Ulcerative colitis should be examined and treated by a doctor to rule out further complications.
What is ulcerative colitis?

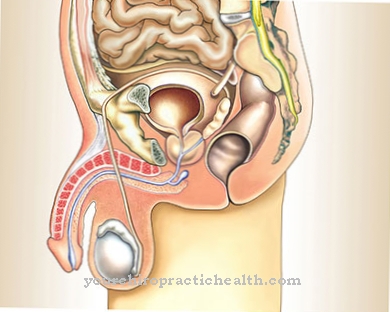
Ulcerative colitis is a chronic inflammatory bowel disease that affects the large intestine (colon). This causes ulcers in the intestinal mucosa, which can extend from the rectum to the transition from the large intestine to the small intestine (ileocecal valve). At this point, the ileocecal valve, the infestation of the intestine ends because ulcerative colitis only affects the large intestine. This is in contrast to another chronic inflammatory bowel disease, Crohn's disease.
Crohn's disease can affect the entire gastrointestinal tract, which differentiates it from ulcerative colitis. The relapses occur again and again in ulcerative colitis and are favored by many factors (stress, poor diet). Even if the disease affects men and women approximately equally, there is a higher incidence of the disease in younger adults.
Despite everything, even small children and older people can be affected. Due to its long-term activity, ulcerative colitis can be a trigger for colon cancer.
causes
The causes of ulcerative colitis are still unknown. A familial, genetic susceptibility is assumed. An autoimmune reaction of the intestinal mucosa to certain substances plays a major role here. This excessive reaction of the mucous membrane is then expressed in the ulcers that are typical of ulcerative colitis.
Evidence was also found that various genetic changes favor the occurrence of the disease. A certain molecular biological protein, the so-called NF-κB transcription factor, is suspected of being permanently active and thus causing ulcerative colitis.
Once the disease is diagnosed, a lifestyle with poor hygiene or other environmental influences can cause the disease to flare up (relapses) constantly. Influences also include diet and living conditions, such as stress, worries and psychological stress.
Symptoms, ailments & signs
In most cases, ulcerative colitis progresses in phases, i.e. phases with severe symptoms alternate with symptom-free intervals. The severity of the symptoms depends on which part of the colon is affected and how advanced the disease is. The main symptom of ulcerative colitis is bloody, slimy diarrhea.
In severe cases, those affected have to struggle with diarrhea up to times a day and also suffer from persistent urge to defecate. Usually, however, the disease begins insidiously with few symptoms and a lower number of diarrhea. Before, during or after a bowel movement, there may be cramp-like pain, especially in the left lower and middle abdomen.
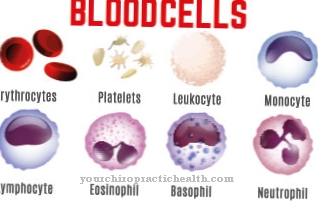
These cramping pains are called tenesmen. The loss of blood through the stool can lead to iron deficiency and anemia, known as anemia. During an acute attack, additional symptoms such as fever, loss of appetite, weight loss, fatigue and physical weakness often occur.
Growth disorders can also occur in childhood. In addition to the symptoms that affect the intestine, ulcerative colitis can also lead to inflammation in organs outside the intestine. Doctors speak of extraintestinal symptoms. Joint problems, eye inflammation, skin changes or inflammation of the bile ducts in the liver can occur.
course
The course of ulcerative colitis can be characterized by frequent relapses and phases of remission (recovery). A distinction is made between acute, severe (fulminant) and chronic attacks. In the latter there is an improvement, but no really symptom-free period (remission). This chronic course usually occurs when the intestine no longer responds sufficiently to the therapy and a higher dosage of the medication is no longer possible due to an intolerance. This makes the course of ulcerative colitis very difficult.
There are different degrees of severity of the course forms. This is the mild course in which only the mucous membrane is swollen. The middle course is characterized by ulcerations (ulcers) and bleeding, but these are not severe.
If the course of the disease is difficult, the intestinal mucosa is inflamed to a greater extent and changes significantly as a result. So-called pseudopolyps and abscesses can develop. The most severe acute form is megacolon (toxic enlargement of the large intestine), which can be life-threatening because of the risk of peritonitis and intestinal perforation.
Complications
Due to the frequent diarrhea, the patients sometimes suffer from massive water, blood and protein losses, which can lead to growth disorders, especially in young people. Ulcerative colitis can also spread to the entire intestinal wall. There is a risk that the intestine will be overstretched and burst.
In addition, it is possible that the inflammation could then appear all over the abdomen, which is known as a toxic megacolon and is extremely dangerous. A toxic megacolon is associated with very severe pain and flatulence, and there is also the risk that bacteria will get into the blood and lead to sepsis (blood poisoning). Bleeding, which can be very severe and life-threatening, can occur as a further complication.
Since the patients can lose a lot of blood in the process, they have to have an operation or have blood transfusions. Furthermore, people who have ulcerative colitis are at greater risk of developing colon cancer, which usually develops about ten to 15 years after ulcerative colitis occurs. In some cases, constrictions or scars also appear in the intestine, which are known as stenoses.
In addition, organs can change pathologically, mainly skin and eye diseases as well as joint inflammation. In rare cases, blood vessels, lungs and heart can also be involved.
When should you go to the doctor?
As with all chronic diseases, diagnosis by a specialist is important. So if permanent diarrhea and bloody stools are observed, going to the internist is inevitable. This also applies when pain in the lower abdomen is almost unbearable. Once the diagnosis has been made, the disease can be treated well. Then it is only up to the person affected how well he can live with it. A strict diet and the use of the prescribed medication lead to a reduction in symptoms.
Not every diarrhea or bloody stool requires medical treatment. If the symptom only occurs for a short time, a visit to a specialist is not necessary. It is then only important that the further course is observed. Spasmodic abdominal pain is also not a compelling sign of ulcerative colitis.
Everyone knows themselves best and knows how to assess the symptoms. If you are unsure or fearful, however, going to the doctor should by no means be postponed. Only he will make the correct diagnosis and, if necessary, start treatment.
Doctors & therapists in your area
Treatment & Therapy
Treatment of ulcerative colitis can be medication and surgery. In addition to mesalazine and sulfasalazine, cortisone is also used, either locally or systemically. To support the intestinal flora, probiotics are given.
Another possibility is the use of immunosuppressors, TNF alpha blockers and biologics as newer forms of therapy. In individual cases with severe attacks, antibiotics can be helpful. In more severe cases, surgical removal of the colon can provide permanent relief.
Outlook & forecast
The prognosis of ulcerative colitis depends on the course of the disease, the general health of the patient and the start of treatment. Ulcerative colitis has a chronic, recurrent or chronically intermittent course in over 80 percent of patients.
In most patients, the disease therefore progresses in phases. There are phases with and without inflammation. In between the attacks, the majority of patients experience a complete recovery and thus their mucous membranes healing. Some patients are completely symptom-free for several years until the next attack.
Ten percent of the sick suffer from a chronically continuous course of the disease. Here the inflammation does not completely subside after the attack. Nevertheless, in particularly severe cases, the prognosis can be very poor. In acute situations, sudden bloody and persistent diarrhea poses a life threat. This increases the risk of death considerably.
In principle, the general cancer risk also increases in patients with ulcerative colitis. The longer a patient has had ulcerative colitis, the higher the likelihood of developing colon cancer as a secondary disease. This significantly reduces the forecast outlook. If the intestine is removed as a result of the disease, the vulnerability to further inflammatory diseases of the intestinal outlet increases.
Aftercare
Regular follow-up care is advisable for ulcerative colitis because those affected can have an increased risk of colon cancer. It can also lead to surgical abscesses or renewed attacks of inflammation. These must be dealt with immediately.
Some ulcerative colitis patients have an increased risk of colon cancer. Statistics show that about five percent of people with ulcerative colitis develop colon cancer later. The risk of developing it depends on the duration of the illness or the areas of the intestine that are chronically inflamed. It is a serious colon disease that lasts for life. Ulcerative colitis repeatedly causes flare-ups.
With each inflammatory flare-up of the colon, a doctor must assess what action to take. Operative measures and post-operative follow-up care are often necessary. Between the inflammatory attacks, immunosuppressants and special nutritional measures can be used to achieve extensive freedom from symptoms. Nevertheless, it is a chronic disease that has far-reaching consequences. This is because other organs can also be affected by the effects of ulcerative colitis.
The attending physicians must also keep an eye on the extraintestinal comorbidities. These can also lead to complications that require treatment. Extraintestinal comorbidities include open skin ulcers, eye infections or biliary problems. Without regular visits to the doctor and expert follow-up care, the sick cannot live symptom-free.
You can do that yourself
Since research into the causes of chronic bowel disease still contains many unfamiliar components, no comprehensive tips for self-help can currently be given.
A stress-free lifestyle is seen as helpful. The focus is on a regular daily routine, adequate rest and recovery phases and a healthy diet. Food intake should be rich in vitamins. Avoid fats and foods that are difficult to digest.
Purification can be used and the intestines should be given enough rest between meals. If there are emotional or mental stress states, it helps to build a stable environment so that a contact person is available at all times. In addition, in these cases the person concerned should not be afraid to see a therapist.
Exercise and sporting activities support well-being as well as a positive attitude towards life. Optimism and confidence are necessary to support the organism. When taking medication, care should be taken to ensure that they do not strain the intestines as much as possible. Pollutants and poisons such as nicotine, alcohol or drugs should also be avoided.
The consumption of chilli or other hot ingredients should also be avoided. The pace of life must be adapted to the possibilities of the person concerned so that unnecessary stressors are avoided. Circumstances in life that are perceived as dissatisfied or stressful must be checked and can be changed or restructured with courage and confidence.

.jpg)

.jpg)






.jpg)

.jpg)
.jpg)











.jpg)