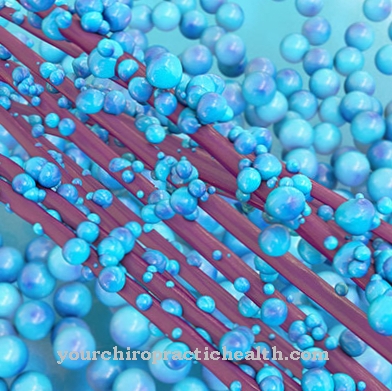
In the eosinophilic granulomatosis with polyangiitis granulomatous inflammation of the small blood vessels occurs. The tissue is traversed by eosinophilic granulocytes.
What is eosinophilic granulomatosis with polyangiitis?

© Tanja Esser - stock.adobe.com
In earlier times, eosinophilic granulomatosis with polyangiitis (EGPA) also as Churg-Strauss syndrome (CSS) known. The pathologists Jakob Churg (1910-2005) and Lotte Strauss (1913-1985) served as namesake. In the present, however, the disease is called eosinophilic granulomatosis with polyangiitis or EGPA for short.
Eosinophilic granulomatosis with polyangiitis (inflammation of the blood vessels) is a rare disease that is one of the ANCA-associated vasculitides (AAV). ANCA is the abbreviation for anti-neutrophil cytoplasmic antibodies. ANCA-associated vasculitis is a systemic disease that can affect almost any organ.
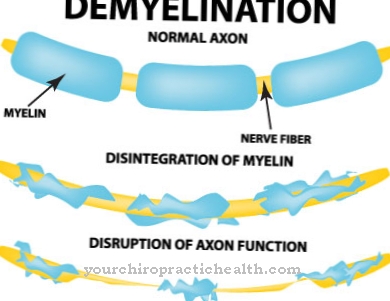
A typical feature of EGPA is involvement of the lungs, which is noticeable through asthma symptoms. In the context of eosinophilic granulomatosis with polyangiitis, a granulomatous (granule-forming) inflammation of small and medium-sized blood vessels occurs. The tissue is infiltrated by eosinophils (inflammatory cells), which are a subset of the white blood cells.
Inflammation of the blood vessels therefore occurs as an immune reaction. Women are twice as likely to develop EGPA as men. In most cases, the disease shows up between the ages of 40 and 50 years. The incidence is one to two new cases per million population each year.
causes
What causes eosinophilic granulomatosis with polyangiitis is still unknown. Various doctors suspect that it is caused by a malfunction of the body's own defense system. Allergic predispositions seem to play a special role.
The EGPA is particularly common in people who suffer from bronchial asthma or other allergies. In addition, the use of certain drugs such as montelukast is considered a risk factor for developing Churg-Strauss syndrome. A striking fact is the fact that the damage to the blood vessels is caused by IgE antibodies. In addition, the disease always begins in the airways, which indicates an immune complex disease.
Symptoms, ailments & signs
The symptoms of eosinophilic granulomatosis with polyangiitis appear in several phases. Chronic respiratory diseases develop at the beginning of EGPA. This can be asthma, an allergic runny nose (rhinitis) or a sinus infection (sinusitis).
While there is an eroded nasal septum in the nose, polyps occur in the sinuses. Bronchial asthma also occurs later. In the second phase of EGPA, blood and tissue eosinophilia takes place. The actual systemic disease only shows up when the vasculitis occurs in the small blood vessels.
In most cases it is accompanied by extravascular granulomas or hypereosinophilia. It has not yet been possible to clarify which factors cause the different phases of the disease. Since eosinophilic granulomatosis with polyangiitis can occur in all organs, the gastrointestinal tract is also affected.
This is noticeable through colic-like symptoms, diarrhea, nausea and vomiting. Furthermore, inflammation of the coronary arteries or the heart muscle is possible, which can lead to cardiac insufficiency or even a heart attack. It is not uncommon for individual nerve damage to be seen, which is accompanied by sharp pain, numbness and paralysis.
If the skin is involved, it will lead to pin-sized bleeding, sores, or ulcers. Other possible temporary symptoms are fever, mild pneumonia, fatigue and weight loss.
Diagnosis & course
The first suspicion of eosinophilic granulomatosis with polyangiitis arises in asthma patients when they suffer from other symptoms such as nerve damage or heart problems. To ensure the diagnosis, tissue samples are taken from the heart region, a nerve or affected areas of the skin.
Vasculitis can be identified by the typical composition of the inflammatory cells. A blood test reveals increased eosinophil granulocyte values, which is a typical finding. Another indication is an accumulation of IgE antibodies. These can be found in around 40 percent of all patients.
Imaging methods such as an X-ray examination, computed tomography (CT) or magnetic resonance imaging (MRI) are used to diagnose foci of disease in the paranasal sinuses, lungs or heart that are not visible. The life expectancy of EGPA patients has been significantly improved in recent years through immunosuppressive treatments.
However, relapses are common, so rigorous monitoring is required. With optimal treatment, the 5-year survival rate is more than 80 percent. However, some patients die from heart attacks or heart failure.
Complications
As a rule, the disease causes symptoms and complications in the respiratory tract. The patient can also suffer from inflammation in the nose and sinuses, which complicate everyday life and reduce the quality of life. Polyps also often develop, which make breathing more difficult.
Due to the reduced oxygen supply, strenuous activities can no longer be carried out and the person affected can lose consciousness. The heart and gastrointestinal tract are also affected, which can lead to heart failure. In the worst case, this can lead to a heart attack and ultimately to death. The general feeling of illness also leads to fever and loss of appetite, which can lead to weight loss. In many cases, pneumonia also occurs.
The treatment is usually causal with the help of antibiotics and is successful after just a few days. However, early treatment is necessary to prevent consequential damage and other complications. There is no reduced life expectancy. Complications can arise if there is a relapse and the patient falls ill with the disease again.
When should you go to the doctor?
If breathing disorders occur, a medical examination should be initiated. If you experience pauses in breathing, shortness of breath, or interruptions in breathing, there is cause for concern. A doctor's visit is necessary, as a persistent lack of oxygen supply to the organism threatens a life-threatening condition. Organ failure can occur, which is associated with irreparable and lifelong damage.
If sleep disturbances occur with simultaneous shortness of breath, a doctor is needed as soon as possible. If you have high blood pressure, problems with the heart rhythm, palpitations, concentration disorders or attention deficits, a doctor should be consulted. Sinus complaints must be examined and treated as soon as they persist for several days or increase in intensity.
If you have symptoms of the stomach or intestines, a doctor's visit is necessary. If nausea, vomiting or diarrhea symptoms occur repeatedly, a doctor should be consulted. In the event of pain, cramps or paralysis all over the body, a doctor must be consulted as soon as possible.
In severe cases, if left untreated, a comatose condition threatens. Numbness of the limbs is considered unusual and should also be evaluated medically. If ulcers form, swelling or a general feeling of illness occurs, a doctor's visit is necessary. In the event of unwanted weight loss, persistent exhaustion or a feeling of physical weakness, a medical examination should be initiated.
Doctors & therapists in your area
Treatment & Therapy
In the early stages of eosinophilic granulomatosis with polyangiitis, the patient is given antibiotics such as trimethoprim or sulfamethoxazole. In addition, anti-inflammatory corticosteroids are given in low doses, which bring about an improvement in two thirds of all patients.
At an advanced stage, patients receive immunosuppressants in addition to corticosteroids. If the course of the disease is severe, the corticosteroid shock treatment is considered to be promising. High doses of corticosteroids are administered in the form of an infusion within a few days. Immunoglobulins can also be used if this treatment is not successful.
If the inflammation can be stopped by administering the medication, the cortisone dose is gradually reduced to the lowest possible dosage. In this way, EGPA can be suppressed permanently in most patients.
Outlook & forecast
The prognosis for eosinophilic granulomatosis with polyangiitis - formerly also known as Churg-Strauss syndrome - varies dramatically. The prognosis is worse, the more organs are affected by the disease. The problem is that this disease can affect practically everyone, mostly in the middle of life.
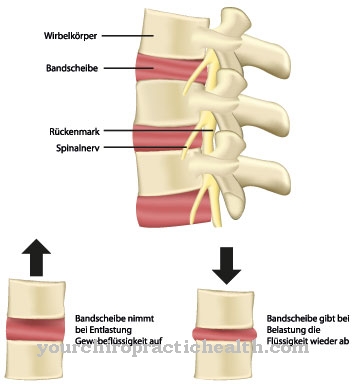
The disease is described by inflamed blood vessels. Only small and medium-sized vessels are affected, but there are many. They lead to the organs and supply them with blood and nutrients. If vital organs such as the heart and brain, the kidneys or the nerves are affected by eosinophilic granulomatosis and polyangiitis, it becomes difficult.
The prognosis is very poor without treatment. It often improves with medical treatment, but only with heavy medication. Corticosteroids or immunosuppressants such as azathioprine, methotrexate or cyclophosphamide are often used.
However, the prognosis for eosinophilic granulomatosis and polyangiitis deteriorates further if these drugs have to be taken for a long time. Such preparations usually have serious side effects. These weaken the already damaged organism even further. If the medication can be stopped slowly because the condition improves, the prognosis will also improve.
Unfortunately, symptoms often come back. These can then be worse from the first outbreak of the disease.
prevention
There are no known preventive measures against eosinophilic granulomatosis with polyangiitis. So the causes of the disease could not yet be determined.
Aftercare
As a rule, there are no special or direct measures and options for follow-up care available to those affected with this disease. Early diagnosis and detection of the disease is primarily important so that other compilations can be avoided. The earlier the disease is detected, the better the further course will usually be.
It is also not possible to heal independently, so that the person affected is definitely dependent on a doctor. The symptoms can only be relieved permanently with proper medical treatment. The disease is usually treated with the help of medication. The person concerned is dependent on the correct dosage and also on the regular intake of the medication in order to alleviate the symptoms.
A doctor should always be consulted if anything is unclear or if you have any questions. They should also be contacted if there are undesirable side effects that have a negative impact on the quality of life of the person concerned. In many cases, contact with other people affected by the disease can also be useful, as it is not uncommon for information to be exchanged. Most of the time, the life expectancy of the person affected is not reduced by this disease.
You can do that yourself
In order not to unnecessarily burden the respiratory tract, the consumption of nicotine should be avoided. Likewise, no rooms should be visited in which there is smoking or other pollutants in the air. To avoid further irritation of the gastrointestinal tract, no toxins such as alcohol should be consumed.
In addition, a healthy diet should be observed and weight loss should be avoided. Sufficient vitamins and fiber promote the recovery process and prevent undersupply. The intake of carbohydrates, animal fats or olive oil should be avoided if possible, as they make the digestive process more difficult. The body needs to be given enough fluids every day to prevent dehydration.
Despite tiredness and exhaustion, it is important that the patient is regularly out in the fresh air and is sufficiently active. To strengthen well-being, activities should be undertaken that promote joy in life.
The exchange with people from the immediate environment also helps to be able to cope with the challenges of everyday life. To reduce stress, it is advisable that the patient use relaxation techniques such as yoga or meditation. The body needs a sufficient supply of heat. We therefore advise against drafts or wearing too thin clothing.



.jpg)

















.jpg)



