The Lyell syndrome is a life-threatening acute skin disease that is associated with extensive epidermolysis (detachment of the epidermis) and can be attributed to a pronounced drug intolerance or an infection with staphylococci. With an incidence of around 1: 1,000,000, Lyell's syndrome is a rare disease.
What is Lyell Syndrome?

© fotoliaxrender - stock.adobe.com
As Lyell syndrome (also "scalded skin syndrome") is a rare, life-threatening acute dermatosis (skin disease) associated with epidermolysis (blistered epidermal detachment) as a result of generalized subepidermal blistering.
In Lyell's syndrome, depending on the underlying cause, there is a distinction between the drug-induced (toxic epidermal necrolysis or TEN), which primarily affects adults, and the staphylogenic variant (staphylococcal scalded skin syndrome), which can be observed especially in infants and young children. differentiated.
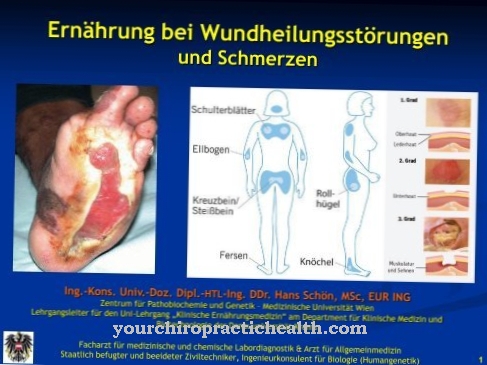
Lyell's syndrome is initially manifested by loss of appetite, inflammation of the mucous membranes (rhinitis) and malaise (prodomal stage). In the acute stage, with persistent fever, generalized blistered erythema (Nikolski phenomenon) and, due to necrosis, develop extensive epidermolysis.
In addition, in many cases the mucous membranes (especially the oral mucosa) are affected by the necrotization.The skin erosions characteristic of Lyell's syndrome lead to a loss of fluid, which can derail the electrolyte and water balance.
causes
The Lyell syndrome is causally due to a pronounced drug intolerance (drug Lyell syndrome) or an infection with staphylococci (staphylogenic Lyell syndrome).
The drug-induced variant of the disease is caused by an allergic-cytotoxic reaction to certain drugs taken. The drugs that can trigger such a reaction include hypnotics (sleeping pills such as barbiturates), non-steroidal anti-inflammatory drugs and analgesics (pain relievers such as pyrazolone derivatives), some antibiotics (e.g. sulfonamides such as cotrimaxol) and anticonvulsants (including anti-epileptics such as carbamazepine, phenotrtoin) and allopurinol (gout remedy) counted.
The staphylogenic Lyell syndrome, on the other hand, is caused by an exotoxin (exfoliatin) produced by Staphylococcus aureus. In many cases the disease is preceded by a purulent skin or conjunctival infection, pharyngitis (inflammation of the lining of the throat) or otitis (inflammation of the ear). While adults usually have an immunity due to antibodies neutralizing the exotoxin, this has not yet developed in infants and small children, so that a staphylogenic Lyell syndrome can manifest as a result of a cytotoxic reaction.
Symptoms, ailments & signs
Lyell's syndrome typically manifests itself as a runny nose, fever, and other flu symptoms. At the same time, those affected feel increasingly exhausted. The appetite decreases as the disease progresses, which can lead to weight loss and deficiency symptoms. In general, the sick are less resilient and withdraw from social life.
Chronic illnesses often affect the mental state and cause, for example, depression or an anxiety disorder. Skin changes can also occur. The visible reddening of the skin is characteristic. This erythema eventually leads to a large-scale detachment of the epidermis.
If Lyell's syndrome is not treated, pneumonia, which is associated with serious symptoms, can develop. In the course of the disease, further symptoms can appear, the type and severity of which depend on the patient's state of health. If the sick person is already weakened by another illness, Lyell's syndrome can cause serious cardiovascular diseases.
Symptoms include sweating, racing heart, nervousness, and panic attacks. In severe cases it can lead to circulatory collapse or even heart failure. Symptoms of Lyell's syndrome appear suddenly and get worse as the disease progresses. If the sick person receives immediate medical attention, the symptoms will subside after a few days to weeks.
Diagnosis & course
In addition to the clinical picture, the Lyell syndrome diagnosed on the basis of a skin biopsy with subsequent histological examination. The finding also serves to determine the specific variant present. For example, in the drug-induced variant, the formation of a gap and detachment can be detected in the entire epidermis, while in the staphylogenic Lyell syndrome a detachment of the stratum corneum (outermost layer of skin) from the stratum granulosum (granule cell layer of the skin) can be observed.
In the differential diagnosis, Lyell's syndrome should be differentiated from coarse-blistered impetigo contagiosa, scarlet fever rash, and Stevens-Johnson syndrome. The drug Lyell syndrome has a mortality of around 30 to 50 percent, whereby this rate can be reduced to 20 percent with consistent and adequate therapy. With early treatment and the absence of possible complications (pneumonia, sepsis), the prognosis of staphylogenic Lyell syndrome is favorable.
Complications
Lyell's syndrome often causes those affected to suffer from fatigue and exhaustion. Furthermore, there is also a loss of appetite and those affected show a significantly reduced resilience. Lyell's syndrome also severely restricts social life, as those affected no longer actively participate in social life.
This can also lead to various psychological complaints or depression. The syndrome also leads to a fever or runny nose. If left untreated, Lyell's syndrome can also lead to pneumonia, which is associated with serious discomfort and complications. The immune system of those affected is weakened by this syndrome, making it easier for inflammations and infections to occur. Contact with the outside world must also be avoided to prevent further infections.
Treatment for Lyell's syndrome is causal and depends on the cause. In the busy cases, the complaints can be treated well, whereby there are usually no particular complications. It is not uncommon for the person affected to be put into an artificial coma if the pain becomes too severe due to the skin changes. Lyell syndrome may also reduce the patient's life expectancy.
When should you go to the doctor?
Flu symptoms such as runny nose or fever indicate an illness that needs to be clarified medically. Affected people are best served by a dermatologist who can diagnose or rule out Lyell's syndrome and then initiate appropriate therapy. Concomitant symptoms such as red spots on the skin, swelling or flare-ups indicate an advanced disease that must be treated immediately. In addition, if the person keeps falling asleep or has open wounds, they must be taken to hospital.
The relatives should observe the sick person closely and call the emergency services in the event of a deterioration in their health. This is especially true if there are signs of sepsis or liver or kidney failure. Since Lyell's syndrome can lead to the death of the patient without treatment, a medical examination is urgently required as soon as the sick person noticeably deteriorates physically or mentally. Due to the high risk of side effects and consequential damage, close consultation with the doctor must be maintained during and after treatment. Lyell's syndrome is treated by a dermatologist, internist or organ specialist, depending on the symptoms.
Treatment & Therapy
If you suspect a Lyell syndrome Immediate intensive medical therapy and consistent monitoring of the person affected are indicated. In addition, the immunocompromised sufferers usually need reverse isolation to protect against secondary infections, through which potential transmission routes as a result of contact with the outside world are prevented.
In the context of symptomatic therapy, the same therapeutic measures are usually used that are used for large-scale burns. This includes close monitoring of laboratory parameters, infusions to compensate for the loss of fluid, electrolytes and protein through the open skin lesions, sterile and antiseptic wound care with possible surgical sanitation of the necrotic skin areas, intensive local care and the patient being placed on an air cushion or water bed to prevent additional pressure-induced detachment of the skin.
If a drug-induced Lyell syndrome is present, all drugs that may have triggered the disease and are not essential for life are discontinued and high-dose glucocorticoids are infused intravenously. For the prophylaxis of further infections or if a superinfection has already occurred, therapy with antibiotics that have a low allergy potential may be indicated.
In the case of staphylogenic Lyell's syndrome, antibiotic therapy with high-dose, semi-synthetic β-lactam antibiotics is in the foreground, while the administration of glucocorticoids is contraindicated. Due to the extremely painful changes in the skin, many sufferers of Lyell's syndrome are also put into an artificial coma.
You can find your medication here
➔ Medicines against redness and eczemaOutlook & forecast
If Lyell's syndrome is treated in a timely manner and there are no complications such as blood poisoning or pneumonia, the prognosis is good. The skin complaints then subside within ten to 14 days. Scars only remain in very rare cases. If Lyell's syndrome is detected at an early stage, the onset of the disease can sometimes be avoided. To this end, the patient is given antibiotics to kill the pathogens. If the treatment is successful, the patient's condition will improve within one to two days.
If left untreated, Lyell syndrome can cause complications such as scarring and nerve damage. The visual changes are then often accompanied by chronic pain. In order to ensure a positive healing process, the patient must be regularly examined by a doctor. The medication may need to be adjusted or specific symptoms treated.
The final prognosis can be made by a specialist who takes into account other factors such as the patient's state of health, family history and any accompanying illnesses. In children, the disease usually clears faster than in adults, who often have the disease for one to two weeks.
prevention
One Lyell syndrome can usually not be prevented. Drug intolerance often only becomes evident when the specific preparation is taken. Sustainable use of medication and precise self-monitoring of the ingestion of potentially triggering substances can reduce the risk of Lyell's syndrome or at least minimize the effects of the disease through an early diagnosis.
Aftercare
The follow-up measures for skin diseases usually depend very much on the precise nature of the disease, so that generally no general prediction can be made. Lyell syndrome must first and foremost be examined and treated by a doctor so that it does not lead to further complications or discomfort.
A high standard of hygiene can also have a positive effect on the course of such diseases. In most cases, these diseases are treated with the use of creams or ointments and medication.
The person affected should ensure regular use and the correct dosage in order to permanently alleviate the symptoms. Regular checks by a doctor are very important. In most cases, Lyell syndrome does not have a negative impact on the life expectancy of those affected.
You can do that yourself
Since Lyell's syndrome is a life-threatening disease, medical treatment and care is essential. Self-help measures can only relate to care and support from relatives.
In the event of drug intolerance, the respective drug should be discontinued or replaced with another after consulting a doctor. Possible symptoms such as fever and fatigue can be counteracted with bed rest and avoiding unnecessary stress. The affected person is usually dependent on an inpatient stay. Loving care by relatives or friends has a very positive effect on the course of the disease. Extensive discussions with close confidants can prevent and treat psychological complaints.
If children are affected by Lyell's syndrome, they should always be informed about the possible consequences and complications of the disease. Furthermore, in many cases contact with other sufferers of Lyell's syndrome also has a very positive effect on the disease. The exchange of information and possible mutual spiritual support should be emphasized here. In general, it is impossible to predict whether this syndrome will be cured.

.jpg)

.jpg)






.jpg)

.jpg)
.jpg)











.jpg)