Escitalopram is a drug that belongs to the group of selective serotonin reuptake inhibitors (SSRIs). It is mainly used in the treatment of depression.
What is escitalopram?
Escitalopram is an antidepressant that belongs to the group of selective serotonin reuptake inhibitors (SSRIs). It is used in the treatment of depression, generalized anxiety disorders, social phobias, and panic and obsessive-compulsive disorders. It increases drive and is also given for pain caused by diabetic polyneuropathy.
Its bioavailability is 80 percent and the plasma half-life is around 30 hours. The maximum effective level is reached after about 4 hours. The application takes place either in the form of tablets or as a solution.
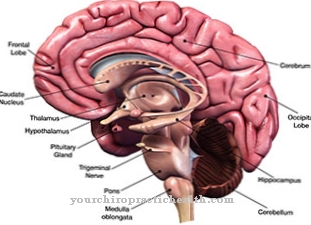
Pharmacological effect on the body and organs
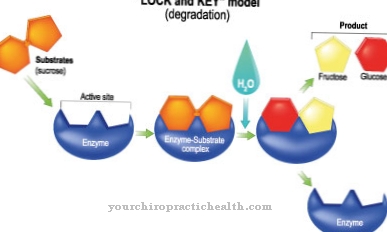
Escitalopram is the chemically active S-form of citalopram (S-enantiomer from the racemate). It works like a selective serotonin reuptake inhibitor.
Escitalopram blocks the transport substances that are responsible for returning the neurotransmitter serotonin to the storage locations after the signal has been transmitted. As a result of this inhibition, more free serotonin is available in the brain for the transmission of nerve signals. This can also explain the mood-enhancing and anti-anxiety effect of escitalopram.
Its effect is comparable to that of citalopram, but occurs much faster. The first improvements can be observed after just one to two weeks of regular use.
Medical application & use for treatment & prevention
So-called endogenous depression (major depressions), panic disorders (with or without agoraphobia), generalized anxiety disorders, obsessive-compulsive disorder and social phobias are considered indicators for the use of escitalopram. It is also used for pain caused by diabetic polyneuropathy.
Furthermore, there is information on the effectiveness of symptoms such as migraines, menopausal symptoms, premenstrual dysphoric syndrome and strokes to improve cognitive performance.
Escitalopram is not suitable for the treatment of children and adolescents. The antidepressant should always be taken exactly as directed by the doctor. Unless otherwise prescribed by the attending physician, the usual dose for adults is 10 mg once a day. The maximum daily dose is 20 mg. Elderly patients take 5 mg escitalopram once a day, an increase should be discussed with the doctor.
No dose adjustment is necessary in patients with mild to moderate kidney dysfunction; in severe kidney dysfunction, the drug should not be used or only after consultation with a doctor. If the patient suffers from mild to moderate liver dysfunction, the daily intake is 5 mg, after 2 weeks the dose can be increased to 10 mg in consultation with the doctor.
The duration of the treatment is determined by the doctor. As with any medicine, the duration of treatment varies with escitalopram. It is not uncommon for a treatment to be successful after a few weeks. However, taking the tablets should not be stopped. In addition, the treatment should be continued for at least 6 months after the symptoms have subsided.
You can find your medication here
➔ Medicines against depressive moods & to lighten the moodRisks & side effects
The very common side effects when taking escitalopram include headache, insomnia, nausea, constipation, lack of strength, tremors, drowsiness, increased sweating and dry mouth.
Often there are also sleep, concentration, memory, sensation, vision, taste or anxiety disorders, fatigue, nervousness, confusion, changes in appetite, weight changes, digestive problems, stomach pain, vomiting, increased salivation, flatulence, hypersensitivity reactions Skin (e.g. rash, itching), muscle pain, impotence and racing heart or a drop in blood pressure.
Occasionally, during treatment with escitalopram, seizures, a slow heartbeat, aggressiveness, an increase in liver values, euphoria, ringing in the ears, allergic reactions (e.g. cough, shortness of breath), fainting or hypersensitivity to light may occur.
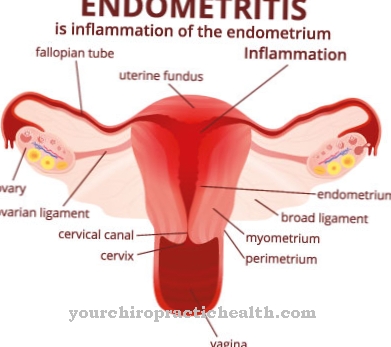
A rare side effect is a decrease in the sodium level in the blood; very rarely, inflammation of the pancreas and liver, skin bleeding, gastrointestinal bleeding, uterine bleeding or even bleeding from the mucous membranes can occur.
Akathisia (restlessness of the limbs) and excruciating restlessness can affect patients, especially at the beginning of treatment. In addition, long-term use of escitalopram can adversely affect the work of cells that build up and break down bones. The result is increased bone fractures or the development of osteoporosis.
Interactions occur with simultaneous intake of escitalopram and MAO inhibitors, tramadol (opioid), alcohol, thiazide diuretics (diuretic drugs), fluvoxamine (SSRI), anticoagulants (anticoagulants), platelet aggregation inhibitors, cimetidine (inhibits gastric acid production) and gastric acid production QT time prolonging drugs.
The use of escitalopram is not indicated in patients who are hypersensitive to the active substance, in patients with severe liver or kidney dysfunction, during pregnancy and breastfeeding, in unstable epilepsy, if there is an increased tendency to bleed, if simultaneously taking MAO inhibitors, if there is a tendency hypokalemia, congenital long QT syndrome (ion channel disease with a pathologically prolonged QT interval in the cardiac current curve) and decompensated heart failure.









.jpg)