Of the Skin fungus or the Dermatomycosis is one of the most common skin diseases in all countries, but this disease is actually easy to avoid. Anyone who is infected should go to the doctor immediately to get rid of the disease as soon as possible.
What is a skin fungus?

© wanchai chaipanya - stock.adobe.com
In dermatology, a skin fungus is also referred to as dermatomycosis or tinea. This is an infection that causes skin disease. The disease manifests itself as itching, reddening and flaking of the affected areas of the skin. It is triggered by certain fungi, which are also called dermatophytes in technical jargon.
There are usually three different types of fungus that cause this disease: trichophytes, microspores or epidermophytes. Trichophytes are the pathogens that are considered to be the cause of fungal skin disease in around 70 percent of cases in Central Europe.
The superficial skin fungus is also known as superficial tinea and can appear on all possible parts of the body. In so-called tinea profunda, the deeper layers of the skin are usually affected by hairy parts of the body, mainly the head and beard area.
causes
For a skin fungus to break out, certain areas of the skin must come into contact with a pathogen. The pathogens penetrate the body, spread around the entry area and cause inflammation of the skin.
Fungal skin on the feet is particularly common. Public buildings in particular, such as swimming pools or open-air pools, in which people walk barefoot and there is a warm, humid climate that favors fungi, are often places where you can easily become infected with skin fungus (or athlete's foot). In addition to floors, contaminated objects can also be the cause of a skin fungus infection.
Animals can also be carriers of fungal diseases. The pathogens pass on to humans when they are stroked or when cleaning cages or brushes. The danger for humans here is that the fungi can often survive for a long time in the horn material of the animals without the animals showing symptoms of the pathogen. People with a weakened immune system are particularly susceptible to skin fungal infections.
Symptoms, ailments & signs
As a rule, skin fungus is associated with very unpleasant complaints, which have a very negative effect on the patient's quality of life and also significantly reduce it. The patients suffer primarily from redness that occurs directly on the skin. This redness spreads over the entire body and thus also reduces the aesthetics of the person concerned.
Many patients therefore also suffer from a significantly reduced self-esteem and inferiority complexes, which can lead to psychological complaints. The redness is often associated with itching, which is only aggravated by scratching. Abscesses can also develop. If the affected person scratches the redness, it can also cause scars.
The skin fungus can also spread to other people if sufficient hygiene is not observed. Patients often lose hair in the affected areas, making these areas appear bare and unsightly. However, the life expectancy of the person affected is not negatively influenced by the skin fungus. There are usually no particular complications with this disease if it is treated in good time. It can also be limited relatively well by means of self-help.
Diagnosis & course
A superficial skin fungus manifests itself as reddened and flaky areas of the skin that are very itchy. Typically, the hair also breaks off on infected skin areas. If the deeper layers of the skin are infected, the pathogens usually spread along the hair roots.
This leads to inflammation with abscesses and accumulations of pus, which later form crusts. The inflamed hair can be easily pulled out and often leads to bald spots. Due to the many easy-to-notice symptoms, diagnosis is often quick to make.
Usually, a skin fungus is diagnosed by examining it with a microscope or using the Wood light method, in which the affected areas of the skin are irradiated with ultraviolet light and the color of the skin areas indicates a disease.
Complications
The skin fungus causes very unpleasant complaints and symptoms on the patient's skin. In most cases, the skin is reddened and itching occurs. This is usually further intensified if the patient scratches the skin.
In the further course abscesses develop. The skin fungus also has a negative effect on the patient's self-esteem and often leads to inferiority complexes. Those affected are often ashamed of the symptoms and are socially excluded. In children, the skin fungus can also lead to exclusion or bullying. Furthermore, the skin fungus can also cause psychological complaints and not infrequently depression.
The affected areas can also be painful, which sometimes affects sleep. The skin fungus usually does not go away if it is not explicitly treated. The treatment itself does not lead to further complications or complaints. With the help of medication, the symptoms can be alleviated relatively well. In some cases, the skin fungus causes hair loss. This can also be stopped with the help of medication.
When should you go to the doctor?
Changes in the skin are often considered unusual and should be monitored. If redness or swelling occurs, a doctor's visit is necessary as soon as it persists for several days. A doctor should also examine whether the changes have spread. In the event of itching or blistering on the skin, a doctor should be consulted, provided this is not caused by a slight insect bite. A dry or easily inflamed skin quality is an occasion for a medical examination.
If there is flaking or the formation of a horny layer in some areas of the body, a doctor's visit is recommended. As soon as your own targeted body care does not bring any improvement, there is a skin disease that should be investigated. The person affected can try to achieve relief from the symptoms with particularly moisturizing cosmetics. If this is not achieved within a few weeks or if the hardening of the skin increases, a doctor's visit is advisable.
In particular, thickened and discolored layers of skin should be examined. If there are cracks in the skin or open wounds, sterile wound care must be provided. Pathogens can enter the organism through the skin and trigger further diseases. Pain in the skin, numbness or sensory disorders should also be examined and treated by a doctor.
Doctors & therapists in your area
Treatment & Therapy
Fungal skin disease will not go away without treatment. Instead, it spreads further and usually leads to contagion from other people. It must therefore be treated medically in all cases.
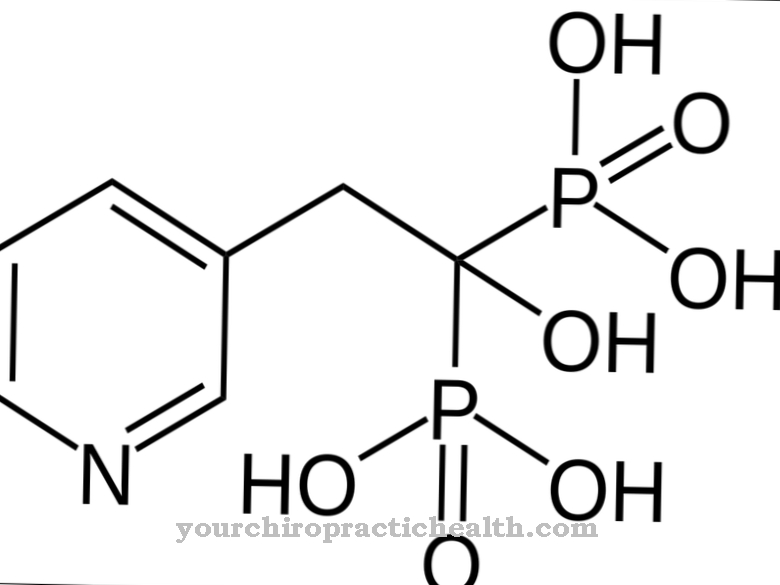
The treatment of a fungal skin disease depends on the type and spread of the skin fungus. If the disease was recognized superficially and relatively early, treatment with an appropriate drug, a so-called antimycotic, which is available in the form of a cream or a liquid solution in the pharmacy, is usually sufficient.
The symptoms of the fungal skin disease are often relieved after hours and the disease is completely healed after just a few days. Treatment of fungal skin diseases of the deeper skin layers, on the other hand, is much more tedious. This requires the administration of a drug that is applied locally to the affected areas, as well as another drug that has to be taken orally over a longer period of time.
This drug then ensures that the pathogens are eliminated from within. Depending on the severity of the disease, treatment can last up to several months. As a rule, however, a cure is possible in all cases; permanent hair loss in the affected areas can only occur if the deeper layers of the skin are infected. In order to ensure successful healing, it is also possible to eliminate any causes of the disease and to take preventive measures in the future.
Outlook & forecast
Skin fungus can be very persistent and will only go away after several months if left untreated in an otherwise healthy person with an intact immune system. However, it often occurs in immunocompromised patients. Since the skin is often poorly supplied with blood anyway and the immune system can therefore only attack there with difficulty, the skin fungus can persist for a very long time in these cases and also spread further. In the worst case, it weakens the immune system so much that it can penetrate further inside the body and attack internal structures and organs.
Treatment with fungicides for oral ingestion and external application helps to cure skin fungus faster and without such consequential damage. However, due to the poor blood flow to the skin, weeks or even months can be expected even with such a treatment. In otherwise healthy patients, the first results can be observed more quickly than in immunodeficient people.
If there are no other health problems besides the skin fungus, even an over-the-counter fundicide as an ointment from the pharmacy can be sufficient; the skin fungus can be treated at home if it is not very common. When the fungicide starts to work, the affected area of the skin will initially become dry and flaky, which deprives the fungus of its livelihood. The visible reddening will then subside and over time the skin will look the same as it did before the fungus erupted.
prevention
There are different ways to prevent fungal skin disease. Walking barefoot should be avoided in public buildings. Wearing flip-flops or flip-flops in swimming pools, saunas, hotel rooms and other places makes sense. There are also sprays and creams on the market that can be applied prophylactically to the feet after swimming.
Especially after swimming or showering, you should make sure that all parts of the body are dried well, including the areas between the toes. Shoes and socks can also be disinfected. When cleaning objects that have come into contact with animals, it is advisable to use a fungicidal disinfectant spray.
Aftercare
A healed skin fungus does not lead to immunity against renewed infection. Former patients have a high degree of personal responsibility to prevent recurring illness. Preventive measures promise remedy. Suitable footwear should be worn in high-traffic and high-risk locations, such as swimming pools and hotel rooms.
Thoroughly dry the skin on the toes, genital area and armpits. However, systematic follow-up care including scheduled doctor's appointments after successful treatment is not provided. As is well known, there are no more complaints.
A fungal infection is often persistent. Patients with chronic immunodeficiency in particular suffer for months or even years. Depending on the severity, certain drugs are used. In mild cases, external treatment is carried out using ointments, sprays or creams. If this therapy does not lead to the desired success, the treating doctor usually prescribes tablets.
In order to replenish the therapeutic resources, the doctor and patient make mandatory appointments. The doctor assesses the course of the disease and, if necessary, takes smears. With the latter, he creates a mushroom culture and can thus adapt the therapy. In the case of stubborn progressive forms, medical support services play a significant role in everyday life. Advice on hygiene rounds off the range of advice.
You can do that yourself
If you suspect a skin fungus, your doctor or a dermatologist should be consulted. Sometimes medical treatment can be supported by various home remedies and self-help measures.
First of all, it is important to dry the skin carefully after bathing or washing. Breathable clothing made of cotton, linen or microfiber reduces perspiration and thus the development of skin fungus. Since the disease is contagious, towels, clothes and bed linen should be washed at over 60 degrees. In addition, there are home remedies such as baby powder or baking powder. Both act against fungi and relieve the unpleasant itching on the skin.
Proven alternatives include coconut oil, garlic, lavender oil or natural yoghurt, which are applied directly to the affected area. Aloe vera also provides quick relief. The remedy relieves itching and at the same time cares for the skin. External and internal use is possible.
In the event of a strong fungal attack, alcohol-based disinfectants can be used. Medical alcohol in the form of disinfectant solutions can also prevent the infection from spreading further. In order to avoid complications such as skin injuries and dehydration, such aggressive agents should only be used after consultation.

.jpg)

.jpg)

.jpg)






.jpg)


.jpg)




