The hepatic encephalopathy is brain damage from metabolic toxins. The cause is liver damage, usually cirrhosis of the liver. Decomposition products, especially ammonia, are no longer adequately disposed of. One of the consequences is hepatic encephalopathy.
What is hepatic encephalopathy?

© juefraphoto - stock.adobe.com
Hepatic encephalopathy is a crisis in the central nervous system caused by liver damage. The body is poisoned by the accumulation of metabolic products in the blood. The pathologically altered liver can no longer break down these “metabolites”. The sensitive nerve cells of the brain in particular suffer from internal intoxication.
The doctors differentiate between 4 degrees of severity according to symptoms:
Grade 1: Reduced ability to concentrate and unstable mood
Grade 2: Extreme tiredness and slight disorientation
Grade 3: Somnolence, speech disorders, severe confusion, motor insecurity and incontinence (spontaneous leakage of urine and stool)
Grade 4: Loss of consciousness and loss of reflexes and pain perception (hepatic coma: coma hepaticum)
root cause
In some textbooks, instead of this 4-stage classification, there is a differentiation between 5 degrees of hepatic encephalopathy. Hepatic encephalopathy is the result of a serious liver disease, primarily advanced liver cirrhosis.
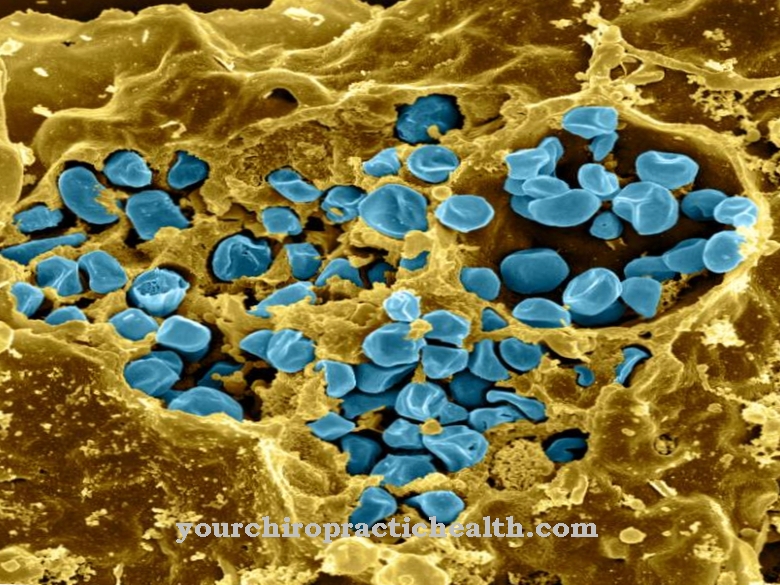
The causes are mostly chronic poisoning of the metabolic organ through excessive alcohol consumption in alcoholism. Intoxication with drugs or other chemicals can also be decisive. In addition, inflammation of the liver (hepatitis) or the bile and bile ducts are the cause of the liver disease.
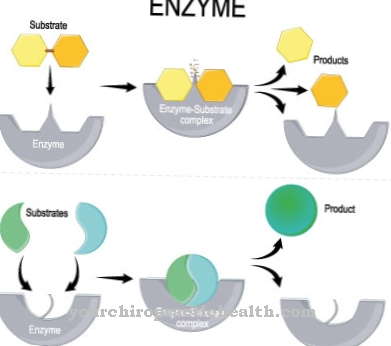
Under the stressful conditions, the liver cannot or can no longer perform its detoxification function sufficiently. The lack of urea synthesis causes ammonia to build up in the bloodstream. There are also other bio-organic compounds such as nitrogenous acids and sulfur compounds. All of these metabolic products have a particularly toxic effect on the brain and lead to the formation of cerebral edema (water retention in the brain).
The result is an increase in intracranial pressure (intracranial pressure) with the result of mental impairments in the context of hepatic encephalopathy.
Symptoms, ailments & signs
Hepatic encephalopathy is characterized by varying degrees of neurological and psychiatric symptoms. In mild cases, there are often no symptoms at all. Or it is a slight decrease in general well-being. With a fully developed hepatic encephalopathy, however, the so-called hepatic coma (coma hepaticum) occurs.
In terms of symptoms, the disease can be divided into four stages or degrees of severity. In stage I, mood swings, sleep disturbances, sometimes euphoric states, slight confusion, eye tremors and slight concentration disorders occur. The symptoms can be so minor that they may not even be interpreted as a sign of illness.
In the second stage of hepatic encephalopathy, the symptoms become more noticeable. Among other things, personality changes, memory disorders, fatigue, disorientation, grimacing and gross trembling of the hands can already occur here. The third stage of the disease is characterized by pronounced sleepiness, severe disorientation, hand tremors and unclear speech.
The patient sleeps all the time, but can still be woken up. In the fourth stage, however, the person concerned can no longer be woken up. This is no longer a question of sleep, but of a comatose state. Symptoms worsen depending on the rate of liver failure.
With acute liver failure, stage IV of the disease is reached quickly. However, chronic liver diseases often also lead to chronic hepatic encephalopathy, which can alternate between severe and mild symptoms.
Diagnosis & course
The symptoms of hepatic encephalopathy are initially unspecific. However, the doctor quickly recognizes from the ammonia level in the blood that there is a hepatic crisis. Nevertheless, other diseases such as sugar shock in diabetes or a stroke must be ruled out in parallel.
Based on the usual liver diagnostics with liver values and sonography as well as computed tomography, the finding is confirmed. An EEG reveals the patient's tendency to have seizures. The classification into 4 stages also describes the possible development as the disease progresses.
Relapses can occur after an acute course of the disease, while chronification often moves into the end stage. The occurrence of death with complete liver failure is also based on hepatic encephalopathy.
Complications
Hepatic encephalopathy results from chronic liver disease. This disease can be harmless, but it can also be life-threatening. The patient may initially appear sleepy and have poor concentration. In further stages, the affected person can fall asleep more and more with increased muscle tension.
This can go on until the person concerned falls into a life-threatening coma (coma hepaticum) with extinguished self-reflexes. Cirrhosis of the liver also has other complications. Its synthesis performance is reduced due to the scarred remodeling of the liver. Fewer proteins are produced than are needed. This leads to a lower oncotic pressure being built up in the blood.
This ultimately results in more water being squeezed out, which in turn leads to edema. The coagulation proteins also decrease, and the patient has a longer bleeding time. Not infrequently there is also a hepatorenal or hepatopulmonary syndrome, which means that the kidneys or lungs can also fail in the course.
Furthermore, the spleen usually enlarges, which causes pain in the left upper abdomen. Varicose veins can develop in the stomach area, which in the worst case can burst and lead to bleeding. The risk of developing liver cancer is also greatly increased in cirrhotic patients.
When should you go to the doctor?
A doctor should be contacted if the person concerned has been suffering from a concentration disorder for a long time. If the usual level of performance drops or if there is persistent lack of drive, a doctor should be visited. If the usual daily obligations can no longer be fulfilled, a doctor should be consulted.
If the person concerned obviously needs help because he can no longer cope with everyday life without care, a doctor must inspect the patient's state of health. Loss of muscle tension, changes in physical appearance, and disorientation are unusual and should be investigated.
Caution should be exercised in the event of impaired consciousness. If there is a loss of consciousness, an emergency doctor should be called. In order to avoid death or lifelong impairment of the patient, first aid measures must be carried out until the emergency services arrive.
Confusion, tremors in the hands or body, and restlessness should be examined and treated by a doctor as soon as possible. A doctor's visit is also necessary in the event of persistent tiredness, fatigue, disturbance of attention or apathy. Involuntary twitching of the muscles, discomfort in the eyes or unsteady gait as well as dizziness are reasons to consult a doctor.
Doctors & therapists in your area
Treatment & Therapy
For therapeutic purposes, hepatic encephalopathy first requires lowering the ammonia level. This is done by specifically influencing the intestinal flora, whereby the proportion of ammonia-producing bacteria is to be reduced.
In addition, the patient receives antibiotics, which mainly work in the intestines, as they are only slowly absorbed. Lactulose, an artificial type of sugar, promotes the growth of lactic acid bacteria, which means that ammonia producers take a back seat. A low-protein diet prevents the intake of excess nitrogen from the outset. For the patient, this means a purely vegetarian diet that does not contain any eggs or milk or any of their processed products.
The doctor achieves support for the liver function through drugs that promote the urea cycle, i.e. the nitrogen elimination. Often the electrolyte balance (minerals) has to be corrected, while the doctor has to prevent an impending desiccosis (dehydration). In addition, the administration of the trace element zinc is appropriate. In some cases, blood plasma cleaning must be carried out (therapeutic plasmapheresis).
Blood flow to the liver can be improved in some of the patients. Affected are people who have had surgical relief of the portal vein in advance. If the blood pressure of the portal vein is surgically raised again, the result is better supply to the liver. In the case of total liver failure, only a liver transplant can help as part of the overall process with the complication of hepatic encephalopathy.
Outlook & forecast
Hepatic encephalopathy can be cured with good and comprehensive medical care. This requires an early diagnosis and the earliest possible start of treatment. In some patients, symptomatic treatment is sufficient to provide permanent relief.
Mood swings or liver dysfunction are alleviated by the administration of medication. The healing process of hepatic encephalopathy is basically described as reversible, provided there are no other disorders and treatment is sought.
Without medical or drug therapy, disease progression is progressive, since no spontaneous healing is to be expected with this disease. The germs spread further in the organism and lead to a deterioration in general health and quality of life. In severe cases, the disease progresses despite treatment.
The ongoing process usually appears with episodic phases. With this clinically manifested hepatic encephalopathy, severe impairments in general lifestyle can be observed. In addition, the patient's risk of death increases significantly.
The poor prognosis in these cases also depends on the underlying disease, the overall diagnosis and the start of treatment. However, the chronic course occurs very rarely. In the case of acute liver failure, there is a risk of the patient's premature death.
prevention
Preventing hepatic encephalopathy means protecting the liver with balanced eating and drinking habits. Alcohol and drug abuse as well as fatty foods affect the central metabolic organ. General food hygiene can prevent hepatitis infections. These measures serve to avoid Liver diseases and ultimately hepatic encephalopathy.
Aftercare
In most cases, the person affected with this disease has no or very few measures and options for direct follow-up care available that can permanently alleviate the symptoms of the disease. In general, an early diagnosis and treatment of the disease has a very positive effect on the further course and can also prevent other complications.
The focus of this disease is therefore on early diagnosis, so that the person affected should consult a doctor as soon as the first symptoms and complaints appear. Treatment for this disease is most often done by taking antibiotics and other drugs. The person affected should always ensure that they are taken regularly and that the dose is correct in order to permanently alleviate the symptoms.
If anything is unclear or if you have any questions, you should always consult a doctor first to prevent further complications. Antibiotics should not be taken together with alcohol, otherwise their effect will be significantly reduced. In many cases, patients are also dependent on the consumption of zinc, although this deficiency can also be controlled through diet. The doctor can create a nutrition plan for the person concerned.
You can do that yourself
Numerous factors precede the changes. The increased intake of proteins is one of the triggers. Likewise dehydration and hypoxia. In chronic hepatic encephalopathy, dietary measures are beneficial.
Likewise, the intake of poorly absorbable antibiotics (e.g. rifaximin) to reduce the ammonia-producing intestinal flora or the intestinal contents. The administration of lactulose is helpful for emptying the bowel. You can influence the reduction in protein content yourself through your diet. Avoiding animal meat is also beneficial.
Hepatic encephalopathy is a sign of poor liver function, which should be positively influenced. Alcohol and sedative drugs should definitely be avoided. The spectrum of changes ranges from slight symptoms to coma hepaticus (liver coma).
In order to better deal with the disease, it is advisable to join a self-help group. The German liver aid is e.g. a non-profit association that was founded by patients 25 years ago. The German Liver Foundation also offers information material and supports the patient, for example in the form of an advice telephone.

.jpg)

.jpg)
.jpg)
.jpg)
.jpg)











.jpg)