The Lentigo maligna is a diffusely limited, flat, brownish-black discoloration of the skin caused by atypical melanocytes. This phenomenon is caused by exposure to the sun and corresponds to a preliminary stage of malignant melanoma. The affected area of skin is completely surgically removed.
What is lentigo maligna?

© scio21 - stock.adobe.com
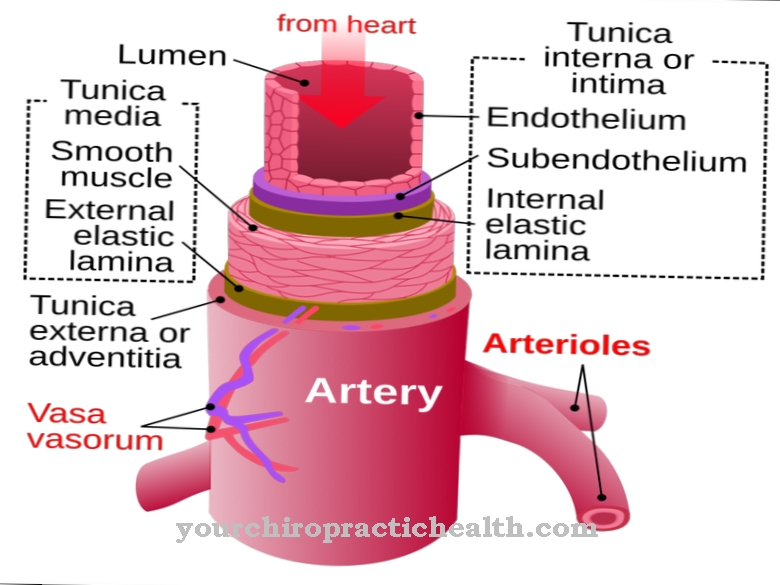
At the Lentigo maligna Atypical melanocytes form in the epidermis. The melanocytes are the cells in the skin that make the pigment and deliver it to the surrounding skin cells. Lentigo maligna is a degeneration process of the pigment-producing cells that takes place in the epidermis of the skin. Degenerate melanocytes are also known as melanomas.
Since the melanocytes in lentigo malignant have not yet become actual cancer cells, but merely appear atypical, the disease can also be referred to as melanoma in situ. The high point of this disease is around 50 years of age. Slightly more women get sick with the phenomenon. Many sources suspect the risk of degeneration of atypical cells at more than 50 percent. Some even suspect that atypical melanocytes always develop into malignant melanoma. However, this development can take several decades.
causes
As a preliminary stage of melanoma, lentigo maligna is an in situ stage of black skin cancer. So far, this disease has mainly been associated with UV radiation. Since the disease has increased in some families, science assumes a genetic disposition as the basis. In this case, the genetic disposition primarily relates to the color of the skin. Well-pigmented people are affected by melanoma far less often than people with genetically light skin.
This is due to the filtering effect of the brown-black melanin. This dark type of melanin is one of two different types of pigment found in human skin. The skin color of every person results from the genetically determined combination of light and dark pigment components. There is more of the dark dye in pigmented people. Studies have shown that this substance renders a high percentage of solar energy harmless.
Symptoms, ailments & signs
Lentigo maligna occurs primarily on skin in the armpits, face, neck and forearms or lower legs. As a rule, the affected skin area is damaged by radiation, so it was already involved in sunburn. Brown to black pigmented and inhomogeneous discolorations of the epidermis are visible on these skin areas.
As a rule, these spots are only diffuse and not raised, but flat.Lentigo maligna can in rare cases also affect the eye. In this context, the phenomenon also appears on pigmented people, since the skin in their eyes is not pigmented. The discoloration is probably related to damage in the DNA of the melanocytes caused by exposure to the sun. In this way, a malignant cell clone of the melanocytes can form in the epidermis. Lentigo maligna usually does not cause pain, itching or other complaints.
Diagnosis & course of disease
The first suspicion of lentigo maligna arises in the context of the anamnesis and visual diagnosis. The suspicion is confirmed histopathologically. In terms of differential diagnosis, the doctor must primarily consider age spots, but also an already mature melanoma that spreads superficially. The prognosis for lentigo maligna promises almost 100 percent healing prospects. Even if lentigo maligna melanoma has already developed, the chances of recovery are still good.
Complications
Treatment is usually necessary for lentigo maligna. Without this, the complaint can develop into skin cancer, which in the worst case can be fatal for the patient. Typically, this disease has various brown areas on the skin. These regions must therefore be completely removed by a surgical procedure.
In many cases, people feel ashamed of the symptoms and feel uncomfortable with the spots or suffer from decreased self-esteem. Furthermore, this disease can also occur in the patient's eye and lead to various visual problems and restrictions in everyday life. It is not uncommon for those affected to suffer from pain on the skin or from itching due to lentigo maligna.
These usually only intensify when the person concerned scratches the respective area. This can lead to bleeding and furthermore to scars on the skin. There are usually no complications with the treatment itself. The affected areas are removed, whereby the patient is still dependent on radiation afterwards. Furthermore, there is usually no reduction in the life expectancy of the patient.
When should you go to the doctor?
Signs of lentigo maligna should always be checked by a dermatologist. Since the skin changes are a preliminary stage of skin cancer, an early diagnosis can possibly save the patient's life. Warning signs such as black discoloration on damaged skin areas therefore always require a comprehensive medical examination. If the areas of the skin suddenly change, this must also be clarified quickly. Bleeding or scarring should also be presented to a doctor. Lentigo maligno occurs mainly in people with a light skin color.
Those who belong to this risk group must ensure that they have adequate sun protection. However, should a sunburn occur, the affected skin area must be monitored by a doctor. If the skin changes mentioned occur, the dermatologist should be consulted. Depending on the cause and severity of the symptoms, the doctor may call in an internist. If mental problems arise as a result of the skin change, this must be discussed with a therapist or as part of a self-help group.
Treatment & Therapy
In lentigo maligna, the affected area is usually completely removed. This process takes place as part of an excision. The affected skin tissue is surgically cut out. Not only is the discoloration completely removed, but also the edges of the adjacent skin areas. Sometimes there is talk of a safety distance. The procedure takes place either under local or general anesthesia.
As a rule, only limited areas of the skin are affected by lentigo maligna. If large areas of the skin are discolored, the defects may be covered with full skin. If the lentigo maligna is in an unreachable position, a laser therapeutic treatment may be preferred. Radiation therapy usually does not take place because this stage is not yet actual cancer.
X-ray irradiation can theoretically be carried out, but should take place with a maximum dose of 100 Gy and only be used in areas that are difficult to reach. The patients appear for follow-up appointments after the operation, during which the recurrence of the skin changes is excluded. Sometimes patients choose not to have the discolored areas removed.
Because of the high risk of degeneration of atypical melanocytes, this approach is not recommended. Melanoma may take years or even decades to develop, but the sooner the atypical cells are removed, the safer it is. For example, hard-to-reach areas of skin can hardly be removed after the degeneration into a lentigo maligna melanoma, since neither laser treatments nor X-rays should take place at this stage.
Outlook & forecast
If left untreated, lentigo maligna shows an unfavorable course of the disease. In further development, skin cancer develops. This endangers the life of the person concerned. If medical help is still not sought despite the increase in symptoms, the person concerned will die from the cancer.
If the diagnosis is made early, an individual treatment plan is drawn up. This provides for the complete removal of the skin changes. The procedure is fraught with complications and side effects. Nevertheless, it is the only possibility that brings with it the prospect of freedom from symptoms. If the operation proceeds without further disturbances or incidents, the lentigo maligna is considered cured. Nevertheless, the patient must take part in regular long-term check-ups in order to be able to take immediate treatment measures if the symptoms recur.
Due to the optical changes, secondary diseases can occur. There is a state of increased emotional distress. This can lead to the development of a mental disorder. When making the prognosis, the possibility of secondary diseases must be pointed out, as these contribute significantly to a worsened outlook. The prognosis is also worsened in patients in whom the skin abnormalities occur in areas of the skin that are particularly difficult to access. Removal in these areas of the body is more complex and may result in not removing all of the diseased tissue.
prevention
Lentigo maligna can be prevented by avoiding direct sun exposure, especially on sensitive skin areas.
Aftercare
As part of follow-up care, it is important to keep the affected areas of skin clean and to avoid skin irritation from clothing or excessive contact as far as possible. In general, after consulting a doctor, a healing ointment containing the active ingredient panthenol can be applied to accelerate the regeneration of the skin. Products containing cortisone should not be used as these would neutralize the inflammatory process required for the treatment of lentigo maligna.
If the skin changes are removed with the help of cryotherapy or surgically, small wounds also remain, which must be protected from contamination and kept dry until they have healed. The most important aftercare measure is lifelong sun protection of the vulnerable areas of the skin with the help of appropriate clothing and sunscreen.
In order to protect the particularly sensitive skin of the head and face, those affected should always wear a sun hat or cap when the sun is shining. Regular self-checks of the skin and biannual to annual check-ups by the dermatologist ensure that new lentigo maligna can be treated at an early stage.
You can do that yourself
People diagnosed with lentigo maligna should have an excision. After such an operation, careful wound care should be taken, as there is an increased risk of infections and wound healing disorders. Should such complications arise, the doctor must be informed. Otherwise the lentigo maligna can recur and possibly even cause cancer.
In addition, those affected should pay close attention to other, mostly unspecific symptoms. For example, pain in the affected area indicates a malignant disease. You should have regular check-ups after surgery to ensure that the skin changes do not recur. Patients who decide not to have the diseased skin area removed should go to regular cancer screening as there is a relatively high risk of degeneration.
In some cases, the discolored areas can be treated with alternative remedies. Citrus acid, for example, has proven itself as it causes the skin to lighten when used regularly. Remedies from homeopathy can also be tried in consultation with the doctor. As a rule, however, the doctor will recommend conservative treatment, which can be supported by the person affected by protection and strict hygiene in the affected areas.








.jpg)
.jpg)
.jpg)







.jpg)