Leukotrienes are substances that are produced in white blood cells, also known as leukocytes, when fatty acids are broken down. Even in small quantities, they are highly effective as mediators in allergic reactions and inflammations.
What are leukotrienes?
The medical name leukotriene already refers to the white blood cells. In the Greek language “leukós” means “white”. Leukotrienes were first discovered in white blood cells.
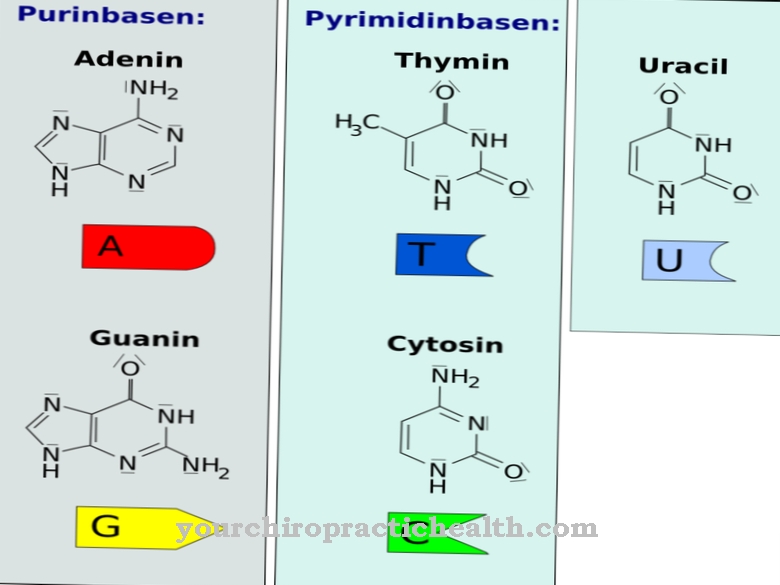
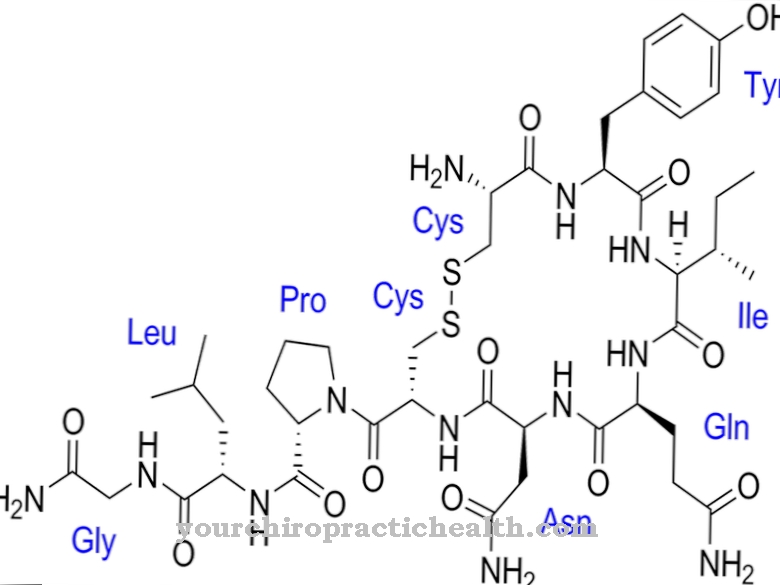
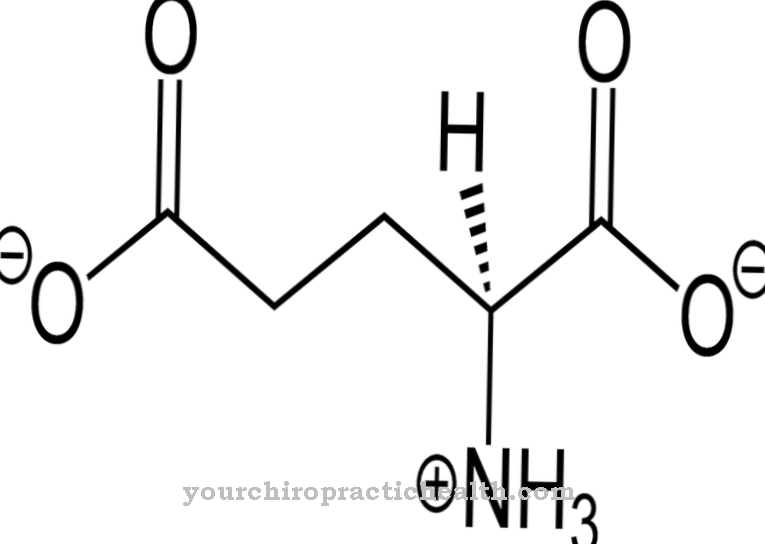
The chemical derivation goes back to arachidonic acid and other polyunsaturated C20 fatty acids. Leukotrienes are highly active biological substances. The biosynthesis is dependent on the enzyme 5'-lipoxygenase. Arachidonic acid reacts in two steps with 15'-lipoxygenase and 5'-lipoxygenase.
Function, effect & tasks
Leukotrienes are derived from arachidonic acid. They are active tissue hormones. They act in the form of mediators that react to inflammatory and allergic reactions by attracting neutrophils.
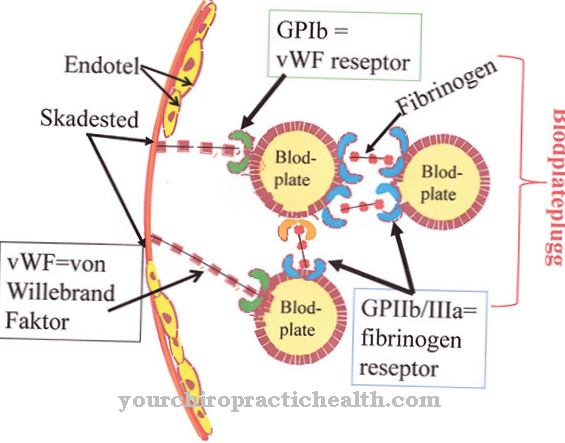
They increase vascular permeability and trigger asthma attacks by means of bronchoconstriction. Leukotrienes have three conjugated triene compounds (double compounds). They belong to the group of substances called eicosanoids. Leukotrienes and prostaglandins are based on arachidonic acid, which is the starting substance. This acid is derived from phospholipids in cell membranes. Inflammatory cells such as mast cells, monocytes, endothelial cells and neutrophils, eosinophils and basophils are able to produce leukotrienes. The synthesis of prostaglandins takes place via the cyclooxygenase. Leukotrienes are created via lipoxygenase. By inhibiting prostaglandins, more arachidonic acid is released to form leukotrienes.
This process creates ASA-induced asthma. Leukotrienes play an important role in inflammatory and allergic reactions in the human body. They are also known as inflammation mediators and are important for the progression of lung diseases. The leukotriene "D4" constricts the airway muscles and increases the production of mucus in the upper airway organs. The bronchi are also affected by this process. There are various leukotrienes with designations such as B, C and D. The cysteinyl leukotrienes "LTC4-LTE4" have a bronchoconstrictor and promote secretion. They are able to trigger anaphylactic or allergic reactions within the lungs. These incidents lead to narrowed airways and thus to asthma attacks.
A chemical stimulus (chemotaxis) causes the leukocytes to adhere to the blood vessel wall. Inflammation is promoted and tissue can be destroyed by superoxide radicals in the course of this process. Leukotrienes interact with interferons and interleukins. At this stage in the course of the disease, leukotriene antagonists, such as montelukast, become active in order to eliminate the undesirable effects on the lungs, airways and bronchi. They block the receptors of the original messenger substance. These unwanted messenger substances occur in the form of stimuli such as house dust, pollen or cold air, which particularly affects asthma patients.
The leukotriene antagonists expand the bronchi, fight inflammation in the lungs and counteract the narrowing of the airway muscles. Symptoms such as coughing, constant tightness and decreased oxygen supply due to breathing problems are reduced and the function of the lungs improved. Leukotriene receptors, which act as antagonists, are used against the suppression of asthmatic, allergic and inflammatory processes in the human body. The first drug of choice is Montelukast Singulair®.
This medication loosens the cramped bronchial muscles and reduces the build-up of mucus in hay fever (allergic rhinitis) and bronchial asthma (bronchial asthma). Small children with intermittent asthma are treated with montelukast in short therapy phases at the beginning of an asthma episode. Most asthma sufferers can live well with their condition while taking this drug. The side effects are usually less than the success of the treatment.
Education, occurrence, properties & optimal values
Leukotriene antagonists are used to treat asthma and allergic rhinitis. In the treatment of asthma, they belong in the field of controllers. Controllers are long-term drugs, they are taken permanently. Leukotriene antagonists compete with glucocorticoid therapy, which is more effective but has more side effects and a greater risk of treatment.
Montelukast may be used as an alternative to glucocorticoid therapy in children up to fourteen years of age if appropriate treatment is indicated. Montelukast is not approved as monotherapy in Germany for people over the age of 15. According to the international guidelines, it may only be used if the attending physician speaks out against glucocorticoid therapy, for example if the patient shows side effects where the damage is rated higher than the expected success of the treatment. Patients who are unable to inhale glucocorticoids are also entitled to alternative treatment with montelukast.
Leukotriene antagonists can also be used in combination with glucocorticoids and beta-2 sympathomimetics (e.g. Ambroxol, Clenbuterol, Bambuterol) in order to achieve a reduced dosage. However, the patient must be an adult. In this therapy, montelukast acts as a so-called "add on". It is not suitable for treating an acute asthma attack. However, it is possible to prevent exertional asthma. Here the preparation works in addition to the basic medication of inhaled glucocorticoids and beta-adrenergic substances (adrenoceptors). These are phylogenetic coupled receptors (GPCR) that are related to the G protein. They are set in motion by the hormone adrenaline.
Diseases & Disorders
Leukotriene antagonists are administered orally in tablet form. They are also available as chewable tablets or granules. These drugs develop their maximum effect around two hours after ingestion.
Despite the possible side effects, montelukast is generally well tolerated. The side effects depend on the individual situation of the patient. These include mental disorders, skin rashes, infections of the upper respiratory organs, gastrointestinal symptoms, muscle and joint pain, Churg-Strauss syndrome (lung and asthma disease) and an increased tendency to bleed.

.jpg)






.jpg)

.jpg)
.jpg)











.jpg)