A Mycosis refers to an infection of living tissue with a fungus. In the Fungal infection it can be about yeast or mold. These can affect either the skin, fingernails and toenails or various organs via the bloodstream. Mycoses can either be harmless and treatable or, in the worst case, life-threatening, depending on which fungus affects which area of the body.
What is mycosis?

© lavizzara - stock.adobe.com
Under one Mycosis Doctors understand living tissue infected by a fungus. The host (which can be a human or an animal or a plant) becomes infected with spores of the respective species of fungus.
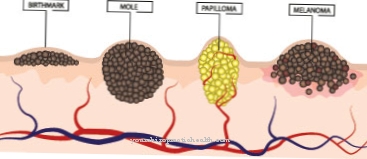
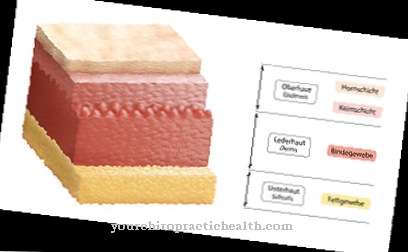
These settle in the body and multiply, causing damage to the affected tissue or even the entire organism. Experts differentiate between superficial and systemic mycoses. The former denote infections of the skin, mucous membrane or nails.
The latter is an attack on the bloodstream and as a result of various organs. While superficial mycoses can usually be treated with medication without any problems, systemic mycoses are potentially fatal and require rapid medical therapy.
causes
The causes of a Mycosis lie in an infection with a fungus. In most cases, spores of the respective species of fungus penetrate the host's tissue.
The spores are parts of the fungus that are capable of growth and that spread in the host. Mycosis in the true sense of the word is only spoken of when it has spread and has caused tissue damage and associated symptoms. In some cases the host's organism succeeds in defending itself against the spread of the fungi; this is known as inapparent infection.
Infection with a fungus can take place in different ways. Among other things, infection from person to person is possible (this is particularly the case with skin and mucous membrane mycoses).
Symptoms, ailments & signs
Systemic mycosis can be severe and ultimately lead to the death of the patient. The systemic form initially causes an increasing fever, which can be associated with a feeling of illness as well as chills, sweating and cardiovascular disorders. This can be accompanied by symptoms such as coughing and shortness of breath.
The main symptom, however, is the skin changes. The person concerned first notices an attack on the skin and nails, occasionally the genital area and face are also involved. The fungus spreads rapidly and over time leads to itching, reddening of the skin and pain. After a few days, the skin begins to flake, which usually makes the itching worse. Large-area lichen planus are also typical.
These can become inflamed and in individual cases cause bleeding or eczema. In the case of a severe course, scars remain, which represent a psychological burden for the sick person, as they mainly appear on visible areas such as arms, legs and hands. Ultimately, the disease leads to respiratory and circulatory failure, from which the patient eventually dies. Early treatment will prevent the fungus from spreading. The skin changes subside after a few days to weeks without any long-term effects or complications to be expected.
Diagnosis & course
A Mycosis is diagnosed in most cases by the attending physician using a sample taken from the affected tissue. A cultivation (rearing) of the pathogen is then carried out from this sample in order to clearly identify it.
Since this method can be quite lengthy under certain circumstances, treatment of the infection is often started in parallel. The doctor decides which therapy is used based on his experience. In addition, a microscopic examination of an infected tissue sample can be carried out to ensure this.
Systemic mycoses generally involve the risk of the host being killed by infecting certain organs. Medical treatment is therefore urgently needed.
Complications
In the worst case, mycosis can also lead to patient death. However, this case usually only occurs if the disease is not treated or if treatment is started very late. In most cases, those affected suffer from fungal diseases that can occur in different parts of the body. The nails and skin are particularly affected.
It is not uncommon for severe itching and flaky skin to occur. Those affected feel uncomfortable with the complaint and are often ashamed of the symptoms. This can lead to depression or other psychological complaints and inferiority complexes. As a rule, the patient's quality of life is significantly restricted and reduced by the mycosis.
The treatment of this disease can be done with the help of medication and usually leads to quick success. There are no particular complications if the mycosis has not affected the internal organs. The life expectancy of the patient is not restricted if the treatment is successful. Adequate hygiene can help prevent fungal infections. Even after successful treatment, the affected person can usually get the same again.
When should you go to the doctor?
If fever, chills, cardiovascular disorders, and other signs of systemic mycosis are noticed, seek medical advice. The infectious disease is a serious condition which, if left untreated, can be fatal.Therefore, a doctor should be consulted at the latest when the characteristic skin changes occur. An infestation of the skin, nails, genital area and face must be examined and treated by a dermatologist. Widespread skin lichens indicate advanced systemic mycosis - a doctor must be consulted immediately.
Regular visits to the doctor are indicated during treatment so that any medication can be regularly adjusted to the rapidly changing symptoms and symptoms. If there is severe itching and other complications, the doctor must also be informed. In addition to the treatment of the physical symptoms, the patient should seek therapeutic treatment to counteract any psychological complaints. Systemic mycosis is treated by the family doctor, the dermatologist and, if necessary, by doctors for internal diseases.
Treatment & Therapy
Does the attending physician have a Mycosis diagnosed, he will initiate appropriate therapy based on the samples taken and his experience.
The exact type of treatment depends on which area of the body is affected and which fungus it is. If the skin of the host is affected, antimycotics (anti-fungal agents) can be prescribed in the form of ointments, which are applied to the respective part of the body. If the mucous membranes are affected, ointments, but also lozenges or suppositories are used (depending on which mucous membrane is affected).
Systemic mycoses are also treated with antifungal drugs; however, in most cases these are given intravenously so that they can act directly in the host's bloodstream. Possible side effects must be weighed against the benefits of a treatment so that the administration of the drug does not cause any more serious damage. In the case of particularly severe or stubborn mycoses, a combination of local and systemic drug treatment is also possible.
Outlook & forecast
If a mycosis is detected and treated early, the prognosis is relatively good. The patients must be treated, but if the therapy is successful they can lead a symptom-free life. The therapy has no long-term consequences for the body and mind, but it can cause short-term complaints that can be a considerable burden. Only treatment with very strong medication can cause permanent organ damage and other physical complaints, which permanently reduce the quality of life and possibly also impair life expectancy.
The prognosis is poor even if the mycosis is well advanced. Aggressive therapy, which is accompanied by various side effects, is often the last possible treatment. The prognosis is accordingly negative. The prognosis for vaginal mycosis, which turns into a chronic disease in five to eight percent of cases, is relatively positive.
Constant medication can alleviate the symptoms and maintain quality of life. The therapeutic treatment with antimycotics is gentle with creams or ointments. Side effects usually do not occur. In the case of systemic mycoses, intravenous treatment is required, which sometimes causes accompanying symptoms such as inflammation.
prevention
In many cases one can Mycosis cannot be prevented directly, as it often occurs indirectly through human skin flakes. The risk of certain fungal infections, for example of the genital organs, can, however, be significantly reduced by not changing partners frequently. If a mycosis is suspected, a doctor should be consulted in any case. This can prevent the infection from spreading and other people in the vicinity.
Aftercare
Follow-up care for a mycosis depends on the type and location of the disease. In the case of small and superficial mycoses, follow-up measures are usually not necessary. This applies especially to not widespread and quickly treated athlete's foot and skin symptoms. With the right therapy, it can be assumed that the fungal infection has been eliminated.
Exceptions are patients who are more susceptible to mycoses due to skin disorders or an immune deficiency. As a precaution, they can also go to a follow-up examination after therapy and have any residues of the fungus tracked down. Superficial mycoses often develop in weak people and damaged skin.
Part of the aftercare should therefore be that the (repeatedly) affected skin areas are kept healthy. In addition, attention should be paid to dryness and a good supply of nutrients. This keeps the skin healthy and the dryness of the spores makes them less likely to nestle. This is especially true for the spaces between the toes and the genital region.
In the case of systemic mycoses, however, follow-up examinations are essential. Any residues and recurring infections must be quickly detected through careful examinations. Prophylactic therapy with antimycotics beyond the treatment period is conceivable.
You can do that yourself
The treatment of mycosis is usually protracted and associated with various symptoms. Those affected can support the healing of the fungal infection by observing strict personal hygiene and following the doctor's instructions.
In consultation with the doctor, various remedies from homeopathy can be used. For example, ointments or suppositories with the active ingredients arnica or belladonna have proven effective. Naturopathy also offers various remedies with marigold ointment and essential oils that alleviate the rash. Which measures can be applied in detail should be decided together with the responsible medical professional.
Strengthening the immune system is generally helpful. This can be achieved through moderate exercise and adequate sleep. If stress is also avoided, the mycosis often heals without complications. However, if further complaints arise, a specialist clinic must be consulted. If the pain increases, professionally guided pain therapy is useful. Since the fungal infection often causes mental suffering, you can speak to a therapist. Patients should contact the doctor for this, who can establish appropriate contacts.
In case of systemic mycosis, hospital treatment is required. Those affected should take appropriate precautionary measures and inform the responsible doctor of any unusual symptoms.

.jpg)
.jpg)
.jpg)







.jpg)

.jpg)
.jpg)











.jpg)