Of the Petroosus major nerve is a nerve pathway in the face and forms a branch of the facial nerve. For the most part it carries parasympathetic nerve fibers, but also some sensory fibers. As part of the parasympathetic nerve, the major petrosal nerve is subject to the action of parasympathomimetics and parasympatholytics.
What is the major petroosal nerve?
The major petrosal nerve is the great petrous nervebelonging to the facial nerve (nervus facialis). It belongs partly to the parasympathetic nervous system, which humans cannot consciously control and which is primarily responsible for calming and regenerative processes. The parasympathetic nervous system is also of great importance for digestive processes.
Other nerve fibers, which also run in the major petrosal nerve, are used to transmit sensory nerve signals. Like all other nerve tracts, the major petrosal nerve is not a smooth structure, but consists of numerous nerve fibers that come together like threads to form a larger bundle. Those threads are the axons of nerve cells and carry electrical signals known as action potentials.
Anatomy & structure
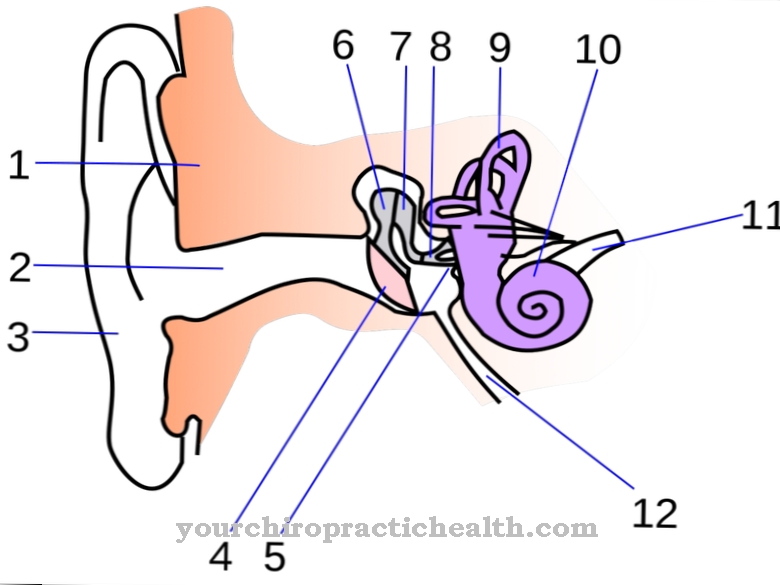
The origin of the major petrosal nerve is the facial nerve or facial nerve. This begins in the brain in the elongated medulla (medulla oblongata) on the upper salivary core (nucleus salivatorius superior). From there it runs through the temporal bone to the geniculate ganglion, which is home to the sensory and sensory cell bodies of the nerve.
The axons of these neurons form the nerve fibers that make up the entire nerve. The major petrosal nerve branches off from the facial nerve and leads through the sphenoid bone (os sphenoidale) to the pterygopalatine ganglion, which is also known as the alar palatal ganglion. In this cluster of nerve cell bodies, the information that the nerve transmits changes to the next (postganglionic) cells. Before the fibers of the major petrosal nerve reach the pterygopalatine ganglion, they converge with the fibers of the deep petrosal nerve.
This nerve carries information from the sympathetic nervous system and begins at the internal carotid plexus; This is a network of nerves on the internal carotid artery or the internal carotid artery. After the pterygopalatine ganglion, the path of the greater petrosal nerve continues through the face to the lacrimal gland, nasal mucosa, nasopharynx and palate.
Function & tasks
The nervus petrosus major represents the connection between the brain and other nerves on the one hand and certain organs in the facial area on the other hand. In the palatal mucosa, the sensory fibers of the nerve are responsible for connecting the taste buds there to the nervous system. They contribute to gustatory perception, although the sensory cells in the palatal mucosa play a subordinate role because of their small number.
Signals from the major petrosal nerve reach the lacrimal gland (glandula lacrimalis) via the lacrimal nerve. It lies diagonally over the eye socket, shifted to the outer side; In addition to liquid, their secretion consists of proteins and electrolytes. Some of the tear fluid reaches the nose via the tear ducts and combines there with other components to form nasal mucus or nasal secretions.
The mucous membrane of the nose is also connected to the petrosal nerve. The nerve does not innervate sensory cells here, but the nasal glands (glandulae nasales). They produce a seromucosal secretion that is part of the nasal mucus. This is made up of various secretions and also includes tear fluid, condensed fluid from the air and mucins from goblet cells. In addition, the major petrosal nerve establishes a neural connection to the nasopharynx (nasopharynx), in the mucous membrane of which there are additional glands.
You can find your medication here
➔ Medicines for paresthesia and circulatory disordersDiseases
Since the major petrosal nerve is part of the parasympathetic nervous system, parasympathomimetics and parasympatholytics can also have an effect on it. These types of drugs are substances that affect the parasympathetic nervous system.
Parasympathomimetics increase the effectiveness of the parasympathetic nervous system. Medicine divides these substances into direct and indirect active ingredients: Indirect parasympathomimetics inhibit the breakdown of neurotransmitters, which trigger a stronger nerve signal with the same amount. Direct parasympathomimetics behave in the synaptic gap like the transmitter acetylcholine. The substance can dock on the postsynaptic receptors and thereby create an action potential in the downstream nerve cell. The neuron does not differentiate between acetylcholine and the parasympathomimetic, but only reacts to the stimulus conveyed by the receptor.
An example of a direct parasympathomimetic is the active ingredient pilocarpine. It stimulates the goblet cells in the airways so that they produce more secretions. It also promotes the formation of tear fluid, for which the major petrosal nerve is also relevant. In addition, pilocarpine leads to increased activity of the pancreas, stomach, intestinal, salivary and sweat glands. Doctors sometimes use the drug against dry mouth that can occur as a result of radiation therapy, as well as in the treatment of glaucoma and pubic lice in the eyelashes. However, the suitability of the drug depends on the individual case.
The pilocarpine iontophoresis sweat test can be used in the diagnosis of cystic fibrosis. Parasympatholytics reduce the effect of the parasympathetic nervous system by competitively inhibiting acetylcholine: the active ingredients occupy the receptors, but do not trigger a reaction. Instead, they only block the receptors for acetylcholine, the release of which is therefore less effective, even though the same amount of neurotransmitters is present. Parasympatholytics are therefore also called anticholinergics. One example of this is atropine, which is used in both ophthalmic medicine and emergency medicine. However, it can also act as a poison and is potentially fatal.



















.jpg)



