As Epidural anesthesia becomes a Spinal anesthesia designated. It is one of the regional anesthesia procedures.
What is epidural anesthesia?

The epidural anesthesia (PDA) is also called epidural (EDA) known. What is meant is regional anesthesia close to the spinal cord. This procedure blocks the transmission of signals such as pain to the spiral nerves. The spiral nerves have their origin in the spinal cord and are located in the intervertebral holes.
To induce spinal cord anesthesia, the attending physician injects a locally acting anesthetic into the epidural space, which is part of the spinal canal. In contrast to general anesthesia, epidural anesthesia only switches off the pain in a localized manner. In principle, the epidural space can be punctured in numerous places. However, the middle area of the lumbar region is considered the safest part of the body. This is where the risk of spinal cord injury is lowest.
Function, effect & goals
The epidural anesthesia is used for various medical purposes. It is considered a tried and tested local anesthetic method during childbirth and provides effective pain relief. It is also used to eliminate pain during a caesarean section. The epidural anesthesia can also be used for surgical interventions in the pelvic region as well as on the legs and feet. Other areas of application are relieving pain after accidents, post-operative pain treatment and the therapy of chronic pain or tumor pain.
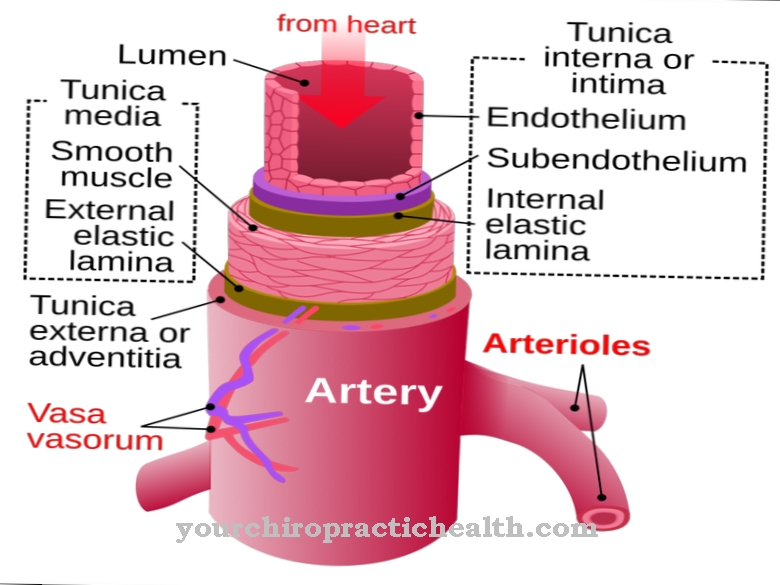
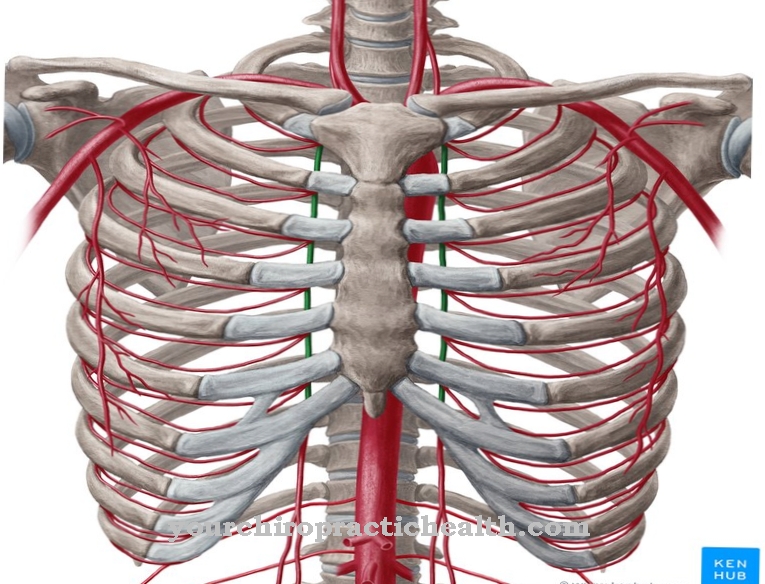
One of the advantages of epidural anesthesia is that it can be used for a long time. In this way, pain medication can be repeatedly introduced into the epidural space via a catheter. The epidural space is also called the epidural space and is part of the spinal canal. Inside the epidural space are the spiral nerves that are blocked by an injected anesthetic. In this way, the transmission of pain can be prevented. After the injection, the local anesthetic is distributed in the epidural space and penetrates to the intervertebral holes. Because the anesthetic has to cross the connective tissue layer of the skin of the spinal cord to be effective, it takes around 20 to 30 minutes to become fully anesthetized.
In contrast to spiral anesthesia, epidural anesthesia can also be used to selectively numb individual areas in the abdominal or chest region. However, a combination of both stunning methods is also possible. In the case of extensive abdominal operations, a combination with general anesthesia is usually used to make the procedure more gentle.
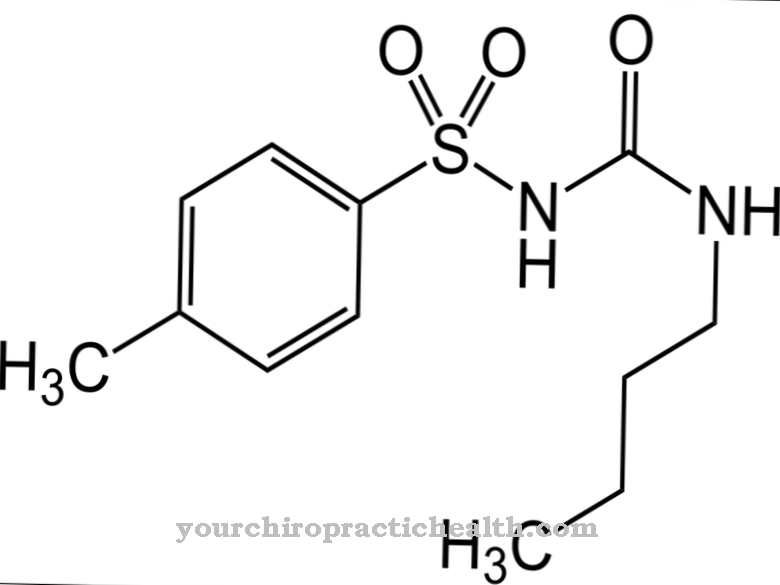
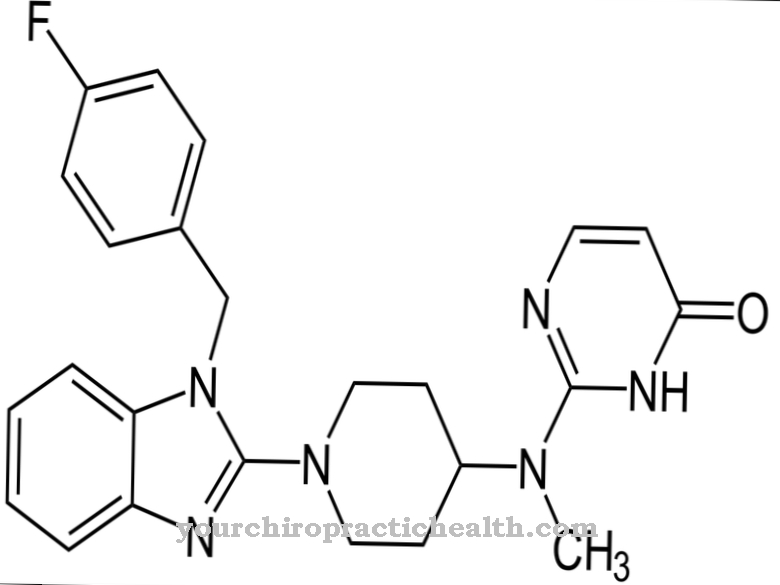
Before the epidural anesthesia, any impairment of the patient's blood coagulation must be excluded. For this reason, the patient must not take any drugs that interfere with blood clotting before the procedure. These include coumarins such as marcumar, clopidogrel and acetylsalicylic acid. In addition, the patient should not consume any solid food six hours before the epidural anesthesia. Drinks must also be avoided two hours before the procedure.
Epidural anesthesia begins with disinfecting and numbing the puncture site. To apply the anesthesia, the anesthetist uses a needle to make a puncture between the vertebrae that extends into the epidural space. As a rule, the puncture takes place between lumbar vertebrae 3 and 4. A puncture between lumbar vertebrae 2 and 3 is also possible. A thin peridural catheter is inserted through the needle. During the procedure, additional painkillers can be administered via catheters.
After the catheter arrives at its destination, the doctor removes the needle again. So that the plastic catheter does not slip, it is fixed with a bandage. A test dose of analgesics is administered to confirm the correct position. The anesthesia first becomes noticeable through a feeling of warmth before the numbness sets in. The anesthetics that are used in epidural anesthesia include: a. Ropivacaine and bupivacaine.
As part of postoperative pain therapy, the patient receives a local anesthetic in a low dose. This procedure does not affect the muscles. In this way, the patient can keep moving without feeling any pain.
You can find your medication here
➔ Medicines for painRisks, side effects & dangers
Epidural anesthesia is considered a relatively safe procedure. When used correctly, complications rarely arise. The risk also depends on the type and amount of narcotics used. These preparations can have different effects on the heart and circulation.
A possible undesirable side effect is the drop in blood pressure during epidural anesthesia. However, the anesthetist prepares for this situation accordingly and counteracts it with medication. Shortness of breath and a slowing of the pulse are also possible.
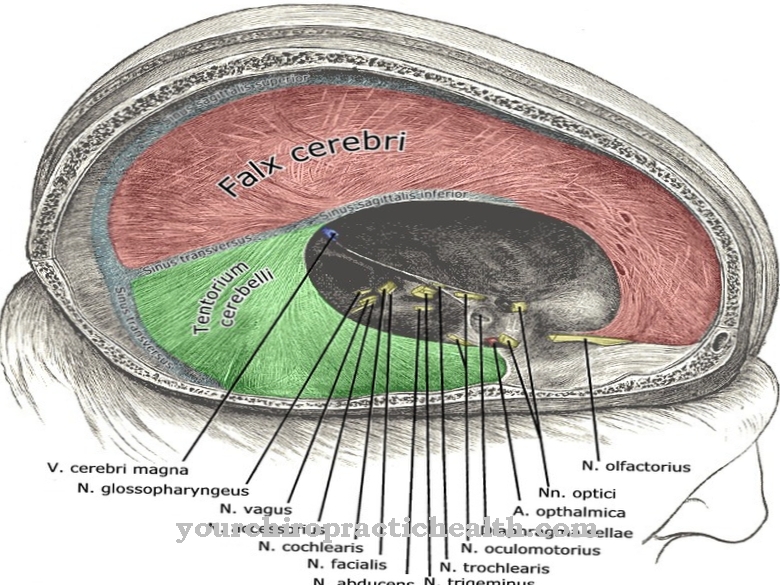
The puncture can also cause complications. These include bruising as a result of a vein injury, an injury to the dura mater (the outermost part of the brain) where nerve water is lost, headache, back pain, or infection. The catheter can also tear off, but this usually has no consequences. Nerve damage from epidural anesthesia is very rare. In this way, the membrane of the spinal cord is not pierced by the needle and catheter. So far, permanent nerve damage has only occurred in isolated cases. Another possible side effect is allergic reactions to the narcotic drug used. However, they also only occur very rarely.
There are also some contraindications that speak against epidural anesthesia. These include infections at the injection site, neurological diseases, blood clotting disorders, narrowing of the spinal canal or shock. Relative contraindications are local diseases of the spine such as joint inflammation, osteoporosis (bone loss), a herniated disc, deformities of the spine, volume deficiency and blood poisoning (sepsis). Furthermore, the consent of the patient is absolutely necessary for this form of anesthesia.












.jpg)
.jpg)
.jpg)







.jpg)