At Pinta it is an infectious skin disease. It occurs only in tropical regions. Due to improved hygienic conditions, however, the number of illnesses has fallen sharply.
What is pinta?

© Peter Hermes Furian - stock.adobe.com
The disease got its name from the Spanish word "pinta", which means spot. In Colombia it also bears the name Carate.
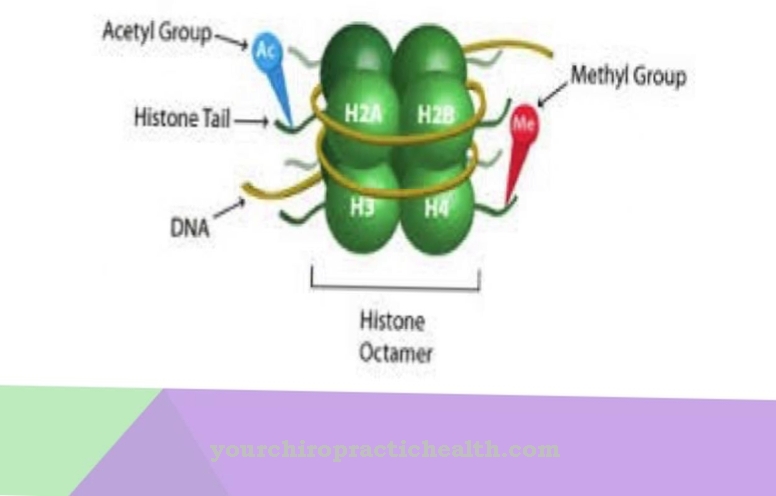
Pinta is a non-venous and endemic treponematosis. It is transmitted by the pathogen Treponema carateum.Treponema is a genus of gram-negative bacteria. You belong to the spirochaetes. This type of bacteria is composed of strange, helical and very mobile cells. They have a scourge that allows them to move quickly. They are also called screw bacteria.
The best-known pathogen of this genus is that of syphilis. The Treponema pathogen was first discovered in Cuba in 1938. The bacterium that triggers the pinta is very similar to that of syphilis. Serologically, the two diseases cannot be distinguished from one another.
causes
Today the causes are scientifically confirmed. However, it was a long process. The pathogen detection turned out to be very difficult. The search for the pathogen was like a tour of discovery like the one that Christopher Columbus had undertaken. In historical writings we can read that a disease of this kind must have existed as early as the Aztec times.
Pinta is an exclusively bacterial infectious disease. The causative agent of Pinta's disease is only native to the tropics. However, just a few decades ago it was spread across the country like an epidemic. These include above all Mexico and other areas in Central and South America.
The screw bacterium is transmitted through direct skin contact with infected people. Open, oozing skin lesions and poor hygienic conditions promote the infection and spread of the pathogen. Young children up to the age of five and young adults between the ages of 15 and 30 are particularly affected. Transmission through sexual contact can largely be ruled out.
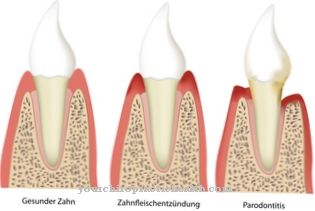
Symptoms, ailments & signs
The symptoms of pinta show up exclusively on the skin. First, papules form on the skin - these are known as primary lesions. They can grow to be several centimeters later. The individual papules merge into one another and increasingly scatter over larger areas. The papules may turn bluish in color.
Depigmentation of the affected skin areas is typical. The onset of tissue shrinkage is also possible. Compared to the related syphilis, there are no bone lesions with Pinta. The cardiovascular system and the central nervous system are usually not attacked by the pathogen.
Diagnosis & course of disease
When the infection begins, Pinta's disease requires an incubation period of two to three weeks. The further course of the disease is divided into three phases:
- In the first stage, reddish lumps appear on the skin. These are still sharply demarcated from one another, slightly raised and not very scaly. They are not prone to swelling or disintegration.
- After five to ten months, the secondary lesion, also known as a pintide, appears. This resembles the primary lesion and occurs predominantly on the extremities and trunk. These papules go into the deeper skin layers and show the typical incipient depigmentation or a bluish discoloration. There is also a swelling of the lymph nodes. Only when the disease persists for several years does a third phase develop.
- The epidermis - the upper layer of the skin - becomes increasingly thick. This process is also called hyperkeratosis. The aforementioned pigmentation disorders are also intensified: these can manifest themselves in overpigmentation (hyperpigmentation) or mostly a strong loss of skin pigments (depigmentation).
The lack of pigments in the skin is reminiscent of the so-called white spot disease Vitiligo, which is one of the autoimmune diseases. In very rare cases, Pinta's disease can lead to long-term cardiovascular effects.
The diagnosis is to be made optically in the contaminated areas. In the early stages, the diagnosis is made with the help of a microscope or a serological examination. In the initial stage it is reminiscent of the yaw bosom or in the later stage of vitiligo.
The similarities to leprosy and psoriasis also make a clear diagnosis difficult. An assignment to the pinta can be made at the latest when the blue color begins and the depigmentation becomes apparent.
Complications
The pinta can cause a number of complications. If the skin disease remains untreated over a longer period of time, the initially small papules increase in size and number and finally merge. This leads to pain, itching and other discomfort. Sometimes there is tissue shrinkage and scarring of the skin. The cardiovascular and central nervous systems are also rarely affected.
If left untreated, the lymph nodes swell and subsequently hyperkeratosis, i.e. a thickening of the upper skin layer. This is accompanied by pigment disorders such as a decrease in skin pigments or hyperpigmentation. Possible long-term consequences of the Pinta are cardiovascular complaints such as cardiac arrhythmias, circulatory collapse or heart attacks. Secondary diseases such as syphilis or ulcus molle can also be favored.
Complications can also arise when treating the pinta. As part of antibiotic therapy, side effects and interactions can occur, which are often particularly intense due to the weakened immune system. The removal of the papules is associated with the formation of scars and immediately leads to profuse bleeding, which often becomes infected and leads to the development of other skin diseases.
When should you go to the doctor?
If unusual skin changes occur after a stay in Mexico or a Central or South American country, a visit to a doctor is recommended. Pinta is a mostly chronic disease that requires lengthy treatment. If you notice the symptoms mentioned, it is best to consult your family doctor or dermatologist. Children, pregnant women, the elderly and people with an immunodeficiency should consult a doctor immediately if the symptoms mentioned occur. The general practitioner, a dermatologist or a specialist in tropical diseases is responsible.
A serious course that manifests itself, among other things, by noticeably light or dark areas of skin, must be examined by a specialist immediately. During therapy, which is medicated, the patient should always consult the responsible doctor due to the high risk of side effects. If gastrointestinal complaints or infections occur, it may be necessary to switch to another preparation. Affected persons ideally keep a complaint diary and keep a record of the course of the disease and the associated symptoms.
Treatment & Therapy
It took decades to localize the pathogen. Today it is known that this chronic infectious disease is a bacterium that responds very well to antibiotic therapy. The treatment is similar to that used for yaws. A single dose of penicillin is usually given for this.
Clinical healing is rapid, especially in the early stages. Alternative antibiotics - such as doxycycline - are available if the patient is intolerant to penicillin. After just 24 hours, those affected are no longer considered to be infectious. The atrophy and depigmentation that exist in the late stages are irreversible. Serological cure is also impossible. Those affected carry the pathogen for life.
You can find your medication here
➔ Medicines against redness and eczemaOutlook & forecast
Pinta is a rare skin disease that offers a relatively poor prognosis. The skin condition is mostly chronic and can persist for years. In severe cases, those affected suffer from Pinta for a lifetime and have to accept various health problems as a result. The quality of life is limited by severe itching and the noticeable pigmentation disorders. Treatment also carries risks. Pinta is usually treated with benzylpenicillin, which can lead to headaches, hair loss and other complaints in the patient.
The outlook and prognosis are based on the severity of the disease. It is provided by an internist who carries out various examinations and also looks at the previous course of the disease. Pinta does not reduce life expectancy. However, as a result of concomitant diseases, further health complaints can occur, which can reduce life expectancy. These include, for example, infections that may lead to blood poisoning.
The prospect of recovery is good if the condition is recognized early, ideally within the three-week incubation period. Then treatment is often possible before the condition develops into a chronic disease.
prevention
The main way to prevent the disease is to follow basic hygiene measures. Since it is a resilient bacterium that is only transmitted through skin contact, direct contact should be avoided. Furthermore, regular, thorough hand washing - this also includes adherence to the exposure time for the soaps and disinfectants used - is imperative.
Aftercare
In most cases, the direct follow-up measures at Pinta are relatively limited. The person concerned is primarily dependent on a quick and above all on early diagnosis of the disease so that no further complications or complaints can occur. The earlier a doctor is consulted, the better the further course of the disease is usually, so that the person affected should see a doctor at the first signs and symptoms.
Most of those affected are dependent on the intake of various drugs at Pinta, which can alleviate and limit the symptoms. The person concerned should always pay attention to the correct dosage and regular intake in order to alleviate the symptoms. When taking antibiotics, it should also be noted that they should not be taken with alcohol.
If anything is unclear or if there are severe side effects, a doctor should always be consulted first. As a rule, Pinta does not need any further follow-up measures after the treatment. The disease does not reduce the life expectancy of the patient, although it can break out again despite treatment.
You can do that yourself
If you suspect Pinta, your family doctor should be consulted first. Depending on the type and severity of the disease, a number of tips and home remedies can be used to accompany medical therapy in order to reduce the symptoms and support the recovery process.
First of all, the doctor will recommend strict personal hygiene. The affected areas must be carefully cared for and disinfected with a medical disinfectant. This prevents the resistant bacteria from spreading further. Regular and thorough hand washing is just as important. The tumors must not be touched or scratched open for the first few days. Patients must choose clothing that does not chafe or stick to the open areas.
This is accompanied by general measures such as exercise, a healthy diet and adequate sleep. If stress is avoided at the same time, the symptoms usually subside quickly. If these measures do not work, the doctor must be consulted. The disease may have another cause that needs to be diagnosed first. The doctor can also give further tips and refer the patient to an alternative practitioner if necessary.




.jpg)

.jpg)




.jpg)



.jpg)