A Thyroid autonomy Along with Graves' disease, it is the most common cause of hyperthyroidism (overactive thyroid) and is characterized by autonomous areas in the thyroid that produce thyroid hormones independently of the hormonal control by the pituitary gland. About 5 percent of the Central European population are affected by thyroid autonomy, with women falling ill more often than men with a ratio of 5: 1.
What is thyroid autonomy?

© Anatomy Insider - stock.adobe.com
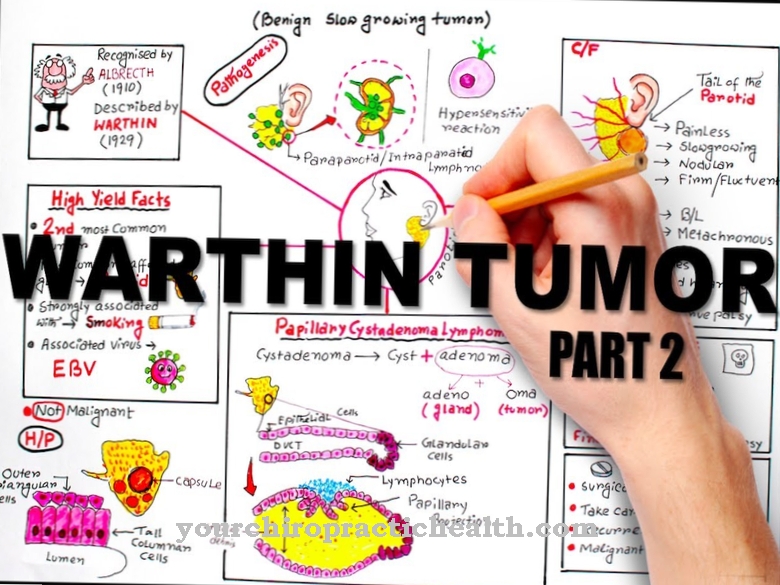
A Thyroid autonomy is a disease of the thyroid gland in which demarcated areas of tissue (adenomas) or the entire tissue have diffusely escaped control by the pituitary gland, so that thyroid hormones are produced uninhibited.
If this autonomous hormone production is above the needs of the human organism, depending on the mass and activity of the autonomic areas as well as the individual iodine intake, initially a subclinical (latent) and later a manifest hyperthyroidism develops, which among other things can manifest through weight loss, tachycardia, psychomotor restlessness as well as diarrhea and menstrual cycle disorders.
In around 50 percent of cases, several areas are affected (multifocal autonomy), in over 30 percent a single area (unifocal autonomy) and in around one sixth the entire thyroid tissue is affected by diffusely distributed cell islets (disseminated autonomy).
causes
A Thyroid autonomy is most often due to an iodine deficiency. Due to this deficiency, the thyroid can no longer produce sufficient hormones and tries to compensate for this by enlarging it (goiter or goiter).
As the stroma increases, the risk of developing nodules that are beyond the control of the pituitary gland and can develop into autonomic areas increases. In addition, unifocal thyroid autonomy can be associated with a mutation of the TSH receptor gene in around 80 percent of cases, which leads to increased growth and increased hormone production by thyrocytes (hormone-producing follicular epithelial cells).
In general, around 30 point mutations are now associated with the development of thyroid autonomy. The striving for autonomy of the affected thyroid tissue is probably also catalyzed by an exogenous supply of high-dose iodine in the form of iodine-containing contrast or disinfectants as well as drugs (including amiodarone), which can also cause the development of hyperthyroidism (overactive thyroid).
Symptoms, ailments & signs
Thyroid autonomy develops extremely slowly and over a long period of time. The symptoms are often only noticed in old age. Typical here is the formation of a nodular goiter, which may also lead to breathing and swallowing difficulties due to the narrowing of the trachea and esophagus.
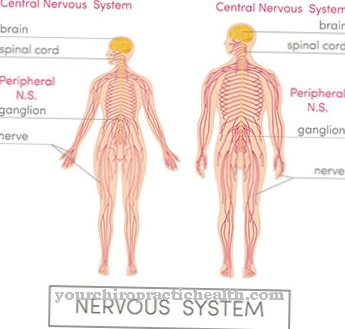
Depending on the functional position of the thyroid gland, symptoms of an overactive thyroid can occur. Thyroid autonomy can therefore be asymptomatic or with significant symptoms. The thyroid hormones are essential for the normal function of cells. In excess, they negatively affect metabolism, which aggravates the functioning of the sympathetic nervous system. This speeds up various body processes and an overdose of adrenaline can be detected in the blood.
Some of these symptoms include nervousness, irritability, increased sweating, racing heart, trembling hands, anxiety, sleep disorders, thinning of the skin, fine, brittle hair, and muscle weakness - especially in the upper arms and thighs. Frequent bowel movements combined with diarrhea can also occur.
Weight loss, sometimes significant, can occur despite a high appetite. Although ten percent of people with an overactive thyroid experience weight gain, vomiting may occur. For women, menstrual flow can vary in frequency and periods, less often or with longer cycles than usual.
Diagnosis & course
Diagnosing a Thyroid autonomy begins in many cases with a determination of the TSH value in the serum in order to rule out hyperthyroidism and to be able to assess the thyroid function. If the TSH value is lowered, the parameters of the peripheral thyroid hormones thyroxine (T4) and triiodothyronine (T3) are usually also determined.
In addition, the thyroid volume as well as morphological or nodular changes can be detected within the scope of a sonography. The diagnosis of thyroid autonomy is finally confirmed by a scintigraphy in which iodine-131 or Tc99m-pertechnetate are administered, which accumulate in the affected thyroid areas and make the affected areas visible in the scintigram. In the differential diagnosis, thyroid autonomy should be differentiated from Graves' disease using an autoantibody test.
Thyroid autonomy is incurable, but has a favorable prognosis if it is diagnosed in good time and therapy is started early. If left untreated, thyroid autonomy with latent hyperthyroidism and excessive iodine intake can lead to a thyrotoxic crisis (life-threatening metabolic disorders).
Complications
Thyroid autonomy can cause a variety of complications. The typical breathing and swallowing difficulties that occur can lead to shortness of breath and aspiration - both of which are associated with further complications. Weight loss can cause dehydration and deficiency symptoms. This leads to a decrease in physical and mental performance, and often also to mental suffering.
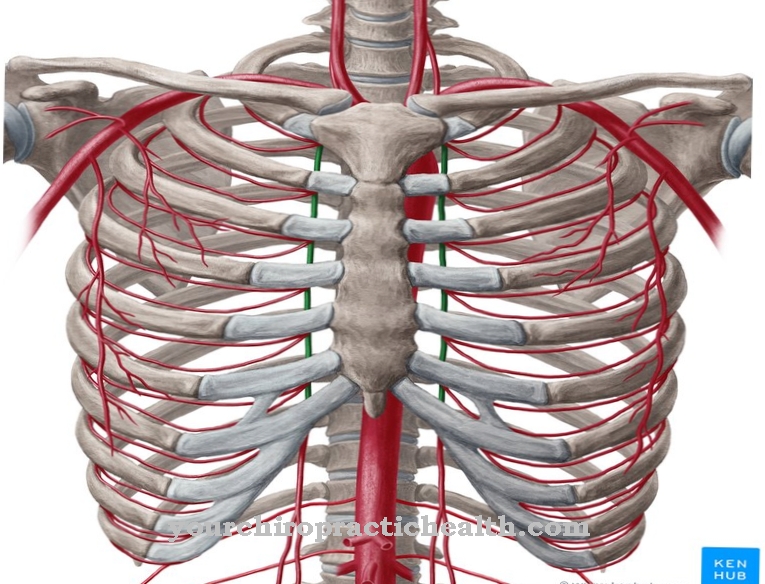
The inner restlessness contributes to the formation of depressive moods and anxiety disorders. If the thyroid autonomy remains untreated, chronic gastrointestinal complaints can develop. Colon cysts form rarely or even stomach cancer develops. At the same time, cardiac arrhythmias can occur which, if the patient has pre-existing conditions, can lead to a heart attack and possibly death of the patient.
The bones can also be damaged in a chronic course - osteoporosis and inflammatory bone diseases occur. Depending on the type of therapy, complications can also arise during treatment. Radioiodine therapy is associated with gastrointestinal complaints and often causes circulatory problems, dehydration and tiredness. Removal of the thyroid can lead to allergic reactions, infections, hoarseness and difficulty swallowing, among other things. Cardiac arrest occurs very rarely.
When should you go to the doctor?
Thyroid autonomy must always be treated by a doctor. It is a serious illness that cannot heal itself. In order to prevent further complications and complaints, a doctor should always be consulted in the case of thyroid autonomy. Early diagnosis and treatment always have a positive effect on the further course of the disease. A doctor can then be consulted if the person concerned has severe difficulty swallowing. This can also lead to breathing difficulties.
In most cases, these symptoms appear for no particular reason and do not go away on their own. Furthermore, an overactive thyroid often indicates thyroid autonomy and should be investigated. Often there is also diarrhea, sleep problems or anxiety. These complaints, too, often point to thyroid autonomy and must be treated by a doctor. A general practitioner can be visited for this. Further treatment is then carried out by a specialist.
Treatment & Therapy
To treat a Thyroid autonomy Various therapeutic measures are available depending on the severity and progression of the disease. If the metabolism is euthyroid (normal hormone production) and there are no clinical symptoms, thyroid autonomy can often be easily observed, whereby prophylactic therapy with levothyroxine or a combination of levothyroxine and iodide should be considered, especially in the case of goiter formation.
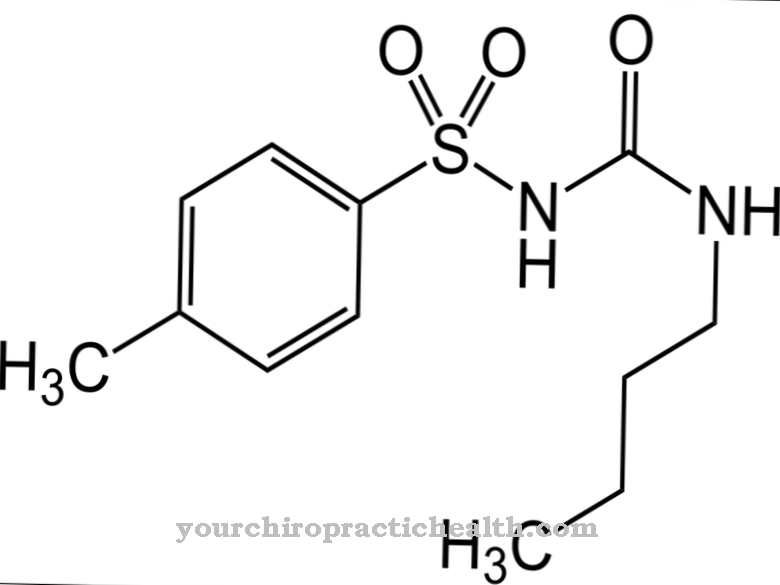
Therapeutic measures are definitely initiated as soon as latent hyperthyroidism is detected, as this can have negative long-term effects on the heart (atrial fibrillation) and bones (osteoporosis). For this purpose, thyreostatics (carbimazole, propylthiouracil, thiamazole) are used, adapted to the individual functional situation, to inhibit hormone production and normalize thyroid function.
Since thyroid autonomy does not show any remissions (regression) and there is an increased risk of thyrotoxic crises, thyreostatic therapy is in most cases only used as a temporary bridge until the definitive form of therapy is selected (radioiodine therapy, thyroid resection), in which the autonomic tissue areas are eradicated, applied.
While the autonomic tissue areas are surgically removed during a resection via an access via the neck, orally administered radioactive iodine-131 usually induces death of the affected person in radio-iodine therapy, which is particularly recommended for multifocal or disseminated forms of thyroid autonomy and goiter formation Tissue.
prevention
There one Thyroid autonomy In most cases this can be traced back to a permanent iodine deficiency, the disease or the growth of the organ and the formation of nodules and goiter can be prevented by a sufficient intake of iodine. A daily amount of iodine of 180 to 200 micrograms is recommended in order to prevent long-term deficiency and thus thyroid autonomy.
Aftercare
Thyroid autonomy promotes hyperfunction. The production of endogenous hormones is disturbed. Physical complaints are the result. The early allocation of iodine preparations counteracts autonomy. Follow-up care is advisable to counteract an overactive thyroid. In addition, the cold nodes must be checked regularly.
Noticeably enlarged tissue or the development of hot nodules requires surgery. The degenerated areas are removed from the thyroid gland. The aim is to stabilize the hormonal balance. The thyroid values should be in the normal range again. Thyroid autonomies lead to weight loss, palpitations and psychological complaints. Difficulty swallowing and breathing are caused by thyroid nodules.
Many patients also complain of a feeling of pressure on the neck. The doctor treats the symptoms with medication. As part of the aftercare, he checks the effect. If necessary, he prescribes more suitable medication or changes the dosage. In the case of thyroid surgery, the well-known postoperative follow-up checks apply. The patient remains in the clinic until discharge.
This also ends the aftercare. Even after a successful operation, the family doctor will check the size of the thyroid gland. Blood tests provide information on the hormone levels. Treatment and aftercare start again when the symptoms return. Any abnormal findings require another operation. Alternatively, iodine therapy can help.
You can do that yourself
In the case of thyroid autonomy, the person affected can strengthen their organism through iodine-containing food. In order to reduce the prevailing iodine deficiency in a natural way, the consumption of algae, cod, haddock or saithe is advisable. In addition, regular consumption of herring, mushrooms or broccoli should be on the menu. Peanuts and pumpkin seeds also help to increase the supply of iodine to the organism.
Meals should also be seasoned regularly with iodized salt. Foods such as spinach and fatty cow's milk also contain an increased proportion of iodine, which can have a positive influence on the course of the disease if the thyroid is autonomous.
However, any intolerance should be checked before consumption in order to avoid complications or side effects. To reduce swallowing difficulties, ensure that the food is sufficiently chewed during the chewing process. The grinding process of the teeth should be optimized and improved. It is important to monitor the weight so that no unwanted weight loss occurs and possible deficiency symptoms can be reduced.
Mental techniques are recommended to reduce anxiety. Autogenic training, meditation or yoga have a strengthening influence on the mental strength of the person concerned. They also reduce stressors and promote well-being.

.jpg)








.jpg)
.jpg)
.jpg)






.jpg)