Splenectomy is a medical term for the surgical removal of the spleen. The procedure is also called Spleen extirpation designated.
What is a splenectomy?

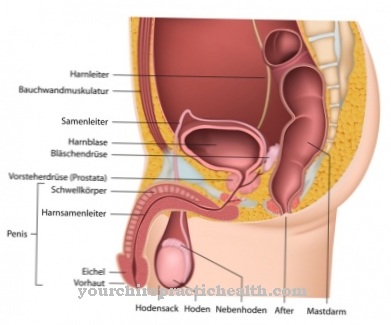
During a splenectomy, the spleen is surgically removed. The spleen is a lymphatic organ that is turned into the bloodstream. It is located in the abdominal cavity in close proximity to the stomach. The spleen performs three functions in the body. On the one hand, there is an increase in lymphocytes in the spleen.
Lymphocytes are white blood cells and are part of the immune system. On the other hand, the spleen is an important storage location for the monocytes. These also belong to the white blood cells. Thirdly, it is used to dispose of and sort out old red blood cells (erythrocytes). In the unborn and in children it also plays a role in the formation of erythrocytes. The spleen is therefore a very well perfused organ. Injury to the spleen can cause life-threatening bleeding. Therefore, the splenectomy is usually an emergency procedure for severe injuries to the spleen that are accompanied by profuse bleeding.
Function, effect & goals
An important indication for a splenectomy is a ruptured spleen. Such a tear in the spleen is usually caused by blunt abdominal trauma. Blunt abdominal trauma can occur, for example, in work or sports accidents. Spontaneous ruptures are rare, but can occur with certain infectious diseases or blood diseases. Spontaneous ruptures are usually preceded by an abnormal enlargement of the spleen (splenomegaly).
The spleen is surrounded by a capsule. If only the capsule is damaged, there is usually only minor oozing bleeding. If the functional tissue is injured at the same time, the bleeding is significantly more severe. In some cases, the bleeding may occur later. If the functional tissue is injured, but the capsule is initially still intact, a bruise develops inside the spleen. With increasing pressure the capsule ruptures and there is sudden heavy bleeding into the abdominal cavity. Such a two-stage rupture of the spleen is an indication for a splenectomy. Non-emergency indications include, for example, hereditary spherocytosis and hereditary elliptocytosis. Hereditary spherocytosis is a congenital hemolytic anemia. Since most of the erythrocytes are abnormal in shape, excessive red blood cells are rejected by the spleen.
As a result, anemia develops. Only by removing the spleen can the excessive breakdown of red blood cells be stopped. The spleen is also removed in autoimmune hemolytic anemia. Thalassemia requiring transfusion is also an indication for surgery. Thalassemia is a disease of the red blood cells. In the past, however, the spleen was removed much more frequently in the presence of thalassemia. Today we try to switch to alternatives. The same applies to the treatment of sickle cell anemia.
If conservative measures fail, the spleen is also removed in idiopathic thrombocytopenic purpura (Werlhof's disease). Further indications for a splenectomy are thrombotic thrombocytopenic purpura (Moschcowitz syndrome) and myelofibrosis in splenic infarction, bleeding, symptomatic splenomegaly or in the case of a high transfusion requirement.
In emergency situations that require quick action, the splenectomy is performed using a generous longitudinal incision in the abdomen. Alternatively, a cross section can be made over the umbilicus. When the spleen is clearly identified as the source of bleeding, the longitudinal incision is widened to the left or the cross-section is widened upward. The source of the bleeding must be identified as quickly as possible and first compressed locally.
After a thorough inspection of the spleen, the decision for the further surgical procedure is made. If the bleeding site is easily accessible, an attempt will be made to stop the bleeding without a splenectomy. If this does not succeed, the splenic hilum is clamped off with clamps. This cuts off the blood supply to the spleen and the bleeding initially comes to a standstill. The spleen is then removed.
In a planned splenectomy, the spleen is usually removed using a left-sided incision on the costal arch. The individual splenic vessels in the splenic hilum are first clamped off and then severed. The organ is then removed. Splenectomy can also be performed laparoscopically as a minimally invasive procedure.
You can find your medication here
➔ Medicines to strengthen the defense and immune systemRisks, side effects & dangers
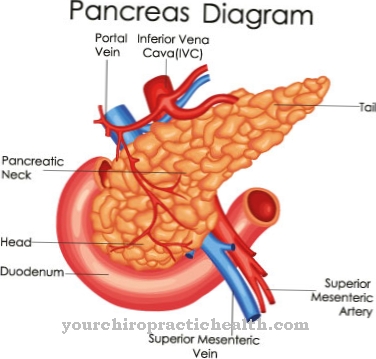
Respiratory complications are more common after a splenectomy. Pneumonia, pleural effusions, and atelectasis can develop. A pancreatic fistula can develop if the tail of the pancreas is lesion (pancreatic tail). After a splenectomy, thromboembolism is also more common. These are caused by the lack of breakdown of the platelets and the resulting thrombocytosis. As a result, 2 to 5 percent of all patients without a spleen suffer a life-threatening thrombosis.
A splenectomy carries a lifelong increased risk of infection. Particularly feared are haematogenic infections with pneumococci, meningococci or Haemophilus influenzae. Post-splenectomy syndrome is a particularly severe form of bacterial infection after a splenectomy. It occurs in 1 to 5 percent of all surgery cases and is associated with a high mortality rate. 40 to 70 percent of all patients with postsplenectomy syndrome die. The cause is a disruption of the phagocytes due to the removal of the spleen, which leads to a reduced defense against encapsulated bacteria.
Post-splenectomy syndrome occurs a few days to several years after the operation. The syndrome is often associated with Waterhouse-Friderichsen syndrome. As a prophylactic measure, patients after a splenectomy are vaccinated against pneumococci, meningococci and Haemophilus influenzae B. Stand-by antibiosis or permanent treatment with antibiotics are also used prophylactically.













.jpg)
.jpg)


.jpg)