Of the Scrotum (scrotum) belongs to the male sexual organs. It consists of skin and muscle tissue and envelops the testicles, epididymis and parts of the spermatic duct and the spermatic cord.
What is the scrotum?
The scrotum is a sac made up of muscle and skin tissue. It is located between the man's legs, below the penis and in front of the perineum. The scrotum is naturally covered with pubic hair. It encloses the testicles and the epididymis. The scrotum probably plays a role in regulating the temperature of the testicles. Various disorders can cause malformations of the scrotum.
Anatomy & structure
Put simply, the scrotum is a skin and muscle pocket that contains the testicles, epididymis and parts of the spermatic duct and the spermatic cord. The skin bag consists of several layers and is divided into two halves by the septum scroti, a separating layer. This separation can also be recognized from the outside and is characterized by the raphe scroti, a line of connective tissue.
The scrotum raphe is also known as the testicle suture. Compared to the rest of the body's skin, the skin of the scrotum is more darkly pigmented. There are many sweat glands on the skin of the scrotum and pubic hair in the unshaven state. In cold temperatures, the skin of the scrotum appears rather thick and wrinkled, in warmer temperatures it can expand and appears smoother. Muscle fibers of smooth muscles and elastic fibers are located under the skin layer. This subcutis is also known as the skin of the flesh (tunica dartos). Inside the scrotum are what are known as the testicle sheaths. A part of these testicular sheaths, the vaginal skin extension, together with a bulging of the peritoneum and the inner trunk fascia, form the testicular cavity (cavitas scroti). The testicles and epididymis are located in this testicular cavity.
The vaginal skin covers the inside of the scrotum, turns inside out and then lies in a second layer on the testicle. A narrow space (cavum vaginale) is formed between the two leaves of the vaginal membrane. This gap allows the testicles to move within the scrotum. The testes are attached to the scrotum via the testicular mesentery, the mesorchium. The testicle is also indirectly anchored to the scrotum via a connection to the epididymis.
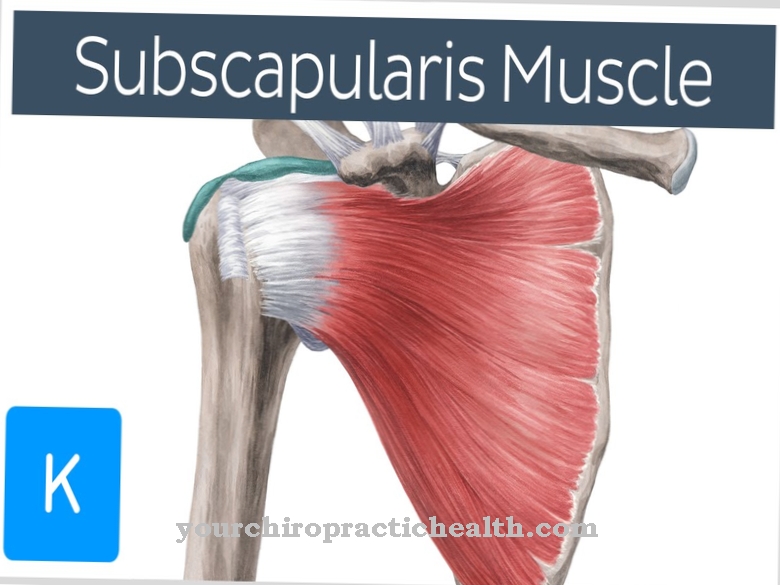
The testicular lifter muscle (Musculus cremaster) consists of fibers from two muscles of the lower abdomen, the Musculus obliquus internus abdominis and the Musculus transversus abdominis. This muscle is innervated by the genital branch and serves as a protective device. When it is cold and touched, the testicular lifter muscle can pull the testicle towards the abdominal wall. The kremaster muscle is also activated when there is strong sexual arousal.
Function & tasks
The exact function of the scrotum has not yet been fully researched. The scrotum probably serves to move the testicle outside of the body cavity. Inside the body, the temperature is too high for the sperm that are formed in the testicles, mature there until they are able to ejaculate and are stored until ejaculation. The temperature in the scrotum is two to five degrees lower than inside the body.
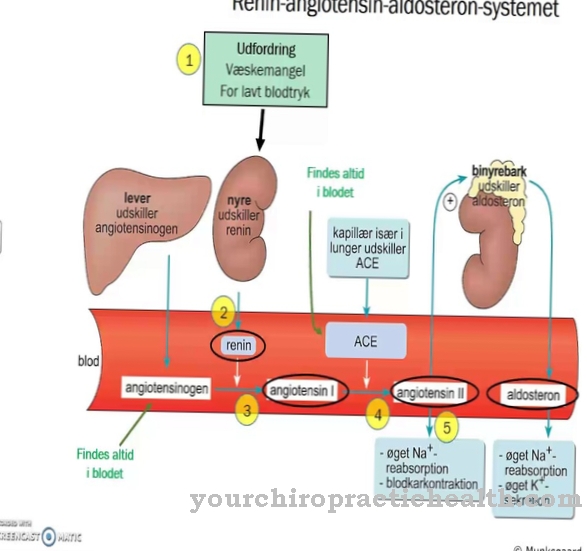
The temperature in the testicle can be adjusted through various mechanisms of the scrotum. When it is cold, the scrotum contracts and shifts towards the abdominal wall. Because of the proximity to the body, the temperature rises here. In addition, the radiating surface for body heat is reduced, not as much heat is lost and the testicles remain warmer. When warm, the scrotum enlarges, so too much heat can be given off better. Testicular arteries and testicular veins also together form a network, which serves as a heat regulator.
Diseases
If the scrotum is completely absent, it is called scrotum agenesis. In most cases, scrotum genesis is associated with anorchia, i.e. a lack of testicular anlage. If the scrotum is only missing on one side, then it is a hemiscrotum. A displacement of the scrotum or half of the scrotum in the region of the groin and perineum is called scrotumectopy. If the scrotum has multiple forms, this is called an accessory scrotum. These malformations and positional anomalies of the scrotum are surgically corrected by removing scrotum tissue or relocating incorrectly applied tissue.
If the venous plexus of the testicle expands, it is called a varicocele or a varicose vein. In 90% of all patients the varicocele is on the left side, in 7% on the right side and in 3% of all patients the varicocele is bilateral. A varicocele can manifest itself as pain or a feeling of heaviness in the scrotum. The varicose vein on the scrotum is caused by a flow disorder of the venous blood. In most cases, the cause of this drainage disorder lies in the abdomen. Often there is a genetic predisposition, especially with right-sided varicoceles, however, a tumor in the abdominal cavity, especially a kidney tumor, should always be considered.
A hydrocele is a swelling of the scrotum as a result of fluid accumulation in the tissue of the skin sac. Hydroceles are mostly genetic, but they can also be caused by infections, trauma or tumors. If necessary, the hydrocele can be surgically removed.
The cremaster muscle is of clinical importance. By brushing the inside of the thigh, a contraction of the kremaster muscle can raise the testicle on the same side. This is known as the cremaster reflex. The cremaster reflex is a so-called external reflex that can usually be triggered in anyone who is healthy. If the testicle does not lift after the inside of the surface has been wiped, this is an indication of damage to the spinal cord segments L1 and L2 or testicular torsion, especially at a young age.








.jpg)

.jpg)
.jpg)











.jpg)